Prioritizing QOL Important to Treating HR+, HER2- Metastatic Breast Cancer
When treating patients with hormone-receptor positive, HER2-negative metastatic breast cancer, mutations necessitate the prioritization of quality of life.
Testing with liquid biopsies can help determine how to treat HR+, HER2- breast cancer.
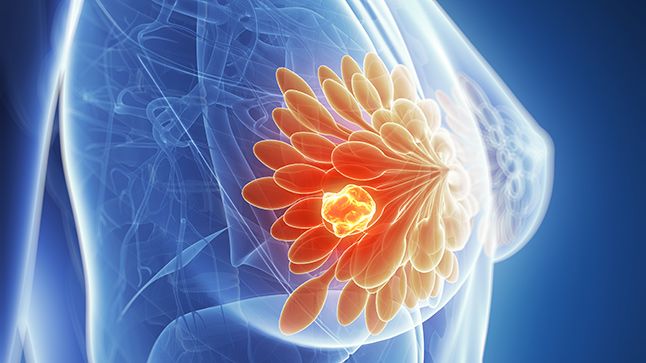
The second-line treatment of mutated hormone receptor (HR)-positive, HER2-negative metastatic breast cancer can become more complex when considering the potential of mutated cancer.
John Novak, PA-C, of the University of Colorado Medicine, led a Community Case Forum with Oncology Nursing News regarding how to address treatment for patients with HR-positive, HER2-negative metastatic breast cancer.
What was the focus of discussion at the forum?
Novak: The overall premise of the forum … was the evolving second-line treatment landscape, and hormone receptor-positive, HER2-negative, metastatic breast cancer. Basically, we focused on how to approach that patient who progresses on first-line endocrine therapy …. And something that's really important is, our people, our providers, doing molecular profiling or molecular testing to determine if patient has a new or acquired mutation that we can potentially target. Two really important targets that are acquired when this type of breast cancer is exposed to endocrine therapy is ESR1 and PI3KCA and both the treatments are a little bit different.
The focus … number 1, is testing being done? … And number 2, if they have an ESR1 mutation, how would you treat that patient? And elacestrant (Orserdu) is an oral selective estrogen receptor degrader that … is indicated for patients who … develop an ESR1 mutation. Then kind of the second thought process was, “OK, if someone has a co-mutation, if a patient has a co mutation, ESR1 mutation and a PI3KCA mutation which target would you focus on?” … Because the treatments are a little bit different. And so patient who has a PI3KCA mutation, per se, would be treated with fulvestrant (Faslodex), which is an injectable SERD, plus alpelisib (Piqray), which is a drug that targets PI3KCA.
How do you decide whether to focus on targeting ESR1 or PI3KCA mutations in treatment?
Novak: One of the big factors is tolerability, or the side effect profile. I think everyone was in agreement that elacestrant is a much better-tolerated medication or treatment overall compared to the PI3KCA inhibitor …. The other factor is that you know elacestrant is an oral drug that you take every day, whereas the other two regimens require a patient to come into clinic every 4 weeks to get an injection in addition to the oral medication that targets PI3KCA.
What should providers know when making treatment decisions about HR-positive, HER2-negative breast cancer with potential mutations?
Novak: The biggest takeaway is doing the appropriate molecular testing or molecular profiling, which is a liquid biopsy, to see if a patient has developed one of these acquired mutations, because that is going to have a huge impact on how we treat that patient. So that would be the most important takeaway, that providers are doing testing with every progression.
The second big takeaway is side effect profile and what everyone was in agreement [about was] if a patient has a targetable mutation, it's much better to go with the treatment that targets that than use something like, say, chemotherapy, or some of the ADCs, which have greater toxicities, even though they may be more effective, like the [antibody-drug conjugates (ADC)] .… They have a lot more side effects… the efficacy data is amazing, but it's also much harder treatment to tolerate.
Why is prioritizing AE profiles important when treating patients with HR-positive breast cancer?
Novak: The treatment of hormone receptor-positive metastatic breast cancer, it's a different beast. It responds very well to anti-estrogen therapies. It's less aggressive, so it's more of a marathon than a sprint. We want to get as much mileage as possible out of the targeted therapies, before going onto something more aggressive, like IV chemotherapy or an antibody-drug conjugate.
… Patients who are on first line treatment, say, with fulvestrant and a CDK4/6 inhibitor, oftentimes they're going to be on that medication for 3-5 years without progressing. And so they're kind of used to being on a treatment that has minimal side effects. There are several good options that we can [use to] target what's driving growth of the cancer, but also kind of minimize these side effects and maintain quality of life, because quality of life is paramount.
This transcript has been edited for clarity and conciseness.
Nurse Practitioners Weigh in on Data From the San Antonio Breast Cancer Symposium
January 16th 2023Loyda Braithwaite, MSN, RN, AGPCNP-BC, AOCNP; and Jamie Carroll, APRN, CNP, MSN, highlight presentations from the 2022 San Antonio Breast Cancer Symposium that will influence oncology nursing practice.



