Power of Palliative Care: How Oncology Nurses Can Increase Referrals
A nurse-driven palliative care referral intervention demonstrated preliminary success in increasing the number of patients who received this form of supportive care.
Palliative care (PC) is fundamental to high-quality cancer care, particularly in the advanced setting. The incorporation of this specialty has been shown to improve quality of life (QOL),1-4 reduce physical and psychological burden, and improve overall survival in some cases of advanced cancer.5-6 Notably, health care organizations such as the American Society of Clinical Oncology (ASCO), the Institute of Medicine, and the National Comprehensive Cancer Network all support the integration of PC into standard oncology care.7-9 However, despite its substantial value, PC continues to be underused throughout the country.10-12
Our outpatient cancer center in Southwestern Pennsylvania is not immune to this trend. While the majority (>94%) of patients treated in our clinical trial unit in 2018 had distant metastasis, only 17.3% had a PC referral. These numbers are in sharp contrast to ASCO guidelines, which recommend that all patients with advanced disease be followed by specialized PC providers while receiving cancer treatment.8
Quality Improvement Initiative
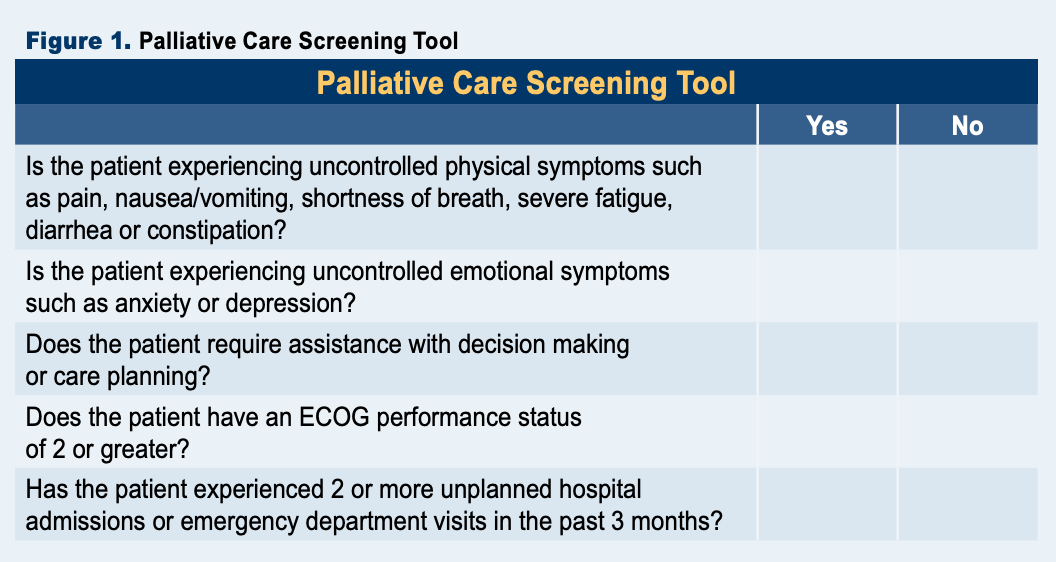
To combat this discrepancy, a nurse-driven PC referral intervention was evaluated in our outpatient clinical trial unit. This intervention included development and delivery of nurse and patient education, creation of an evidenced-based PC screening tool, and establishment of a formal procedure for nurse-led PC referrals.
The procedure for nurse-driven PC referrals included all patients visiting the unit for oncologic treatment. Treatment nurses determined if the patient was already supported by a PC specialist. If a nurse identified a patient who was not receiving PC, they would consequently fill out the PC screening tool (Figure 1). Patients who screened positively on the tool received verbal and written PC education from the nurse, and if they demonstrated interest in PC, they were connected with the PC clinic located in the cancer center.
Education for treatment nurses was delivered by the author during a 30-minute inservice on the nursing unit. The education focused on the purpose and benefits of PC; potential patient, clinician, and institutional barriers; strategies for effectively discussing the specialty; and introduction to the procedure for nurse-driven PC referrals. This information was provided verbally and reinforced with written materials. Reeducation and one-on-one coaching were periodically provided throughout the quality improvement study period. The education provided to the nursing staff served to improve the verbal education they provide to patients. Patient education was also improved through the distribution of a flyer discussing PC and highlighting resources available at the outpatient cancer center.
The final component to this intervention was the development of a tool to assist treatment nurses with the identification of oncology patients in urgent need of PC. The screening tool was developed by the author with assistance from a PC nurse practitioner. The tool consisted of 5 ‘yes’ or ‘no’ questions. An answer of ‘yes’ to any of the questions indicated the patient was especially likely to benefit from a PC referral. The criteria for these screening questions were extracted from a systematic review and international consensus panel of oncology and PC providers.13,14 Special attention was taken to select screening criteria that were readily evaluable and within the nursing scope of practice to assess.
In addition to support from literature, the last 2 screening criteria were also found to be relevant to our population based on locallevel data. In previous logistics regressions, ECOG Performance Status of 2 or greater— and 2 or more hospital admissions or emergency department visits—were shown to predict which patients within our unit were at high risk for dying within the next 90 days.
Figure 1.
Intervention Results
The nurse-driven PC referral project was trialed over a 2-month period. At the end of the trial period, the average percentage of patients followed by PC in the unit increased from 16.4% to 37.6%. During this time, there were 62 unique patients treated, of which 50 were not currently followed by PC and thus eligible for screening. Of these 50 patients, 11 (22%) screened positively on the PC screening tool and were subsequently provided PC education. Six of these patients (54.4%) were interested in PC services and scheduled with the PC clinic. A weekly breakdown of PC use is provided on the previous page (Figure 2).
Overall, the nurse-driven PC referral project was well received by patients and nursing staff. Nurses found the education helpful in making their PC conversations with patients more effective. In addition, they found the process of connecting patients with PC services to be a rewarding experience.
Patients also appreciated the chance to learn about resources available to them, even if they did not ultimately choose to pursue PC at the time. One particularly grateful patient who opted to begin PC services stated, “I am so glad you mentioned this. I am so relieved to know that I don’t have to continue suffering every day.”
Figure 2.

Future Implications
After the preliminary success during the trial period of this nurse-driven PC referral project, the PC screening tool and procedures were implemented as a permanent process for this unit. Leadership also plans to implement these changes throughout other units in the cancer center. To facilitate this change in process, the PC screening tool was also integrated into the electronic medical record.
REFERENCES
1. Temel JS, Greer JA, El-Jawahri A, et al. Effects of early integrated palliative care in patients with lung and GI cancer: a randomized clinical trial. Am J Clin Oncol. 2017;35(8):834-841. doi:10.1200/jco.2016.70.5046
2. Vanbutsele G, Pardon K, Van Belle S, et al. Effect of early and systematic integration of palliative care in patients with advanced cancer: a randomised controlled trial. Lancet Oncol. 2018;19(3):394-404. doi:10.1016/s1470-2045(18)30060-3
3. Zhuang H, Ma Y, Wang L, Zhang H. Effect of early palliative care on quality of life in patients with non-small-cell lung cancer. Curr Oncol. 2018;25(1):54-58. doi:10.3747/co.25.3639
4. Zimmermann C, Swami N, Krzyzanowska M, et al. Early palliative care for patients with advanced cancer: a cluster-randomised controlled trial. Lancet Oncol. 2014;383(9930):1721-1730. doi:10.1016/ s0140-6736(13)62416-2
5. Bakitas MA, Tosteson TD, Li Z, et al. Early versus delayed initiation of concurrent palliative oncology care: patient outcomes in the ENABLE III randomized controlled trial. Am J Clin Oncol. 2015;33(13):1438-1445. doi:10.1200/ jco.2014.58.6362
6. King JD, Eickhoff J, Traynor A, Campbell TC. Integrated onco-palliative care associated with prolonged survival compared to standard care for patients with advanced lung cancer: a retrospective review. J. Pain and Symptom Manage. 2016;51(6):1027-1032. doi:10.1016/j.jpainsymman.2016.01.003
7. Institute of Medicine of the National Academies. Dying in America: Improving Quality and Honoring Individual Preferences Near the End of Life. Washington, DC: The National Academies Press; 2015.
8. Ferrell BR, Temel JS, Temin S, et al. Integration of palliative care into standard oncology care: American Society of Clinical Oncology Clinical Practice Guideline update. Am J Clin Oncol. 2017;35(1):96-112. doi:10.1200/jco.2016.70.1474
9. National Comprehensive Cancer Network. Palliative Care (Version 2.2021). Accessed November 1, 2021. https://www. nccn.org/professionals/physician_gls/pdf/palliative.pdf.
10. Goldwasser F, Vinant P, Aubry R, et al. Timing of palliative care needs reporting and aggressiveness of care near the end of life in metastatic lung cancer: a national registrybased study. Cancer. 2018;124(14):3044-3051. doi:10.1002/ cncr.31536
11. Michael N, Beale G, O’Callaghan C, et al. Timing of palliative care referral and aggressive cancer care toward the end-oflife in pancreatic cancer: a retrospective, single-center observational study. BMC Palliat Care. 2019;18(1). doi:10.1186/ s12904- 019-0399-4
12. Osagiede O, Colibaseanu DT, Spaulding AC, et al. Palliative care use among patients with solid cancer tumors. J Palliat Care. 2018;33(3):149-158. doi:10.1177/0825859718777320
13. Hui D, Meng YC, Bruera S, et al. Referral criteria for outpatient palliative cancer care: a systematic review. Oncologist. 2016;21(7):895-901. doi:10.1634/theoncologist.2016-0006
14. Hui D, Mori M, Watanabe SM, et al. Referral criteria for outpatient specialty palliative cancer care: an international consensus. Lancet Oncol. 2016;17(12):552-559. doi:10.1016/ s1470-2045(16)30577-0
Shared Model of Care Post-HCT Offers Safe Follow-Up, Reduces Patient Burden
Published: March 19th 2025 | Updated: March 19th 2025Alternating post-HCT care between specialized facilities and local cancer centers produced noninferior non-relapse mortality and similar quality of life to usual care.


