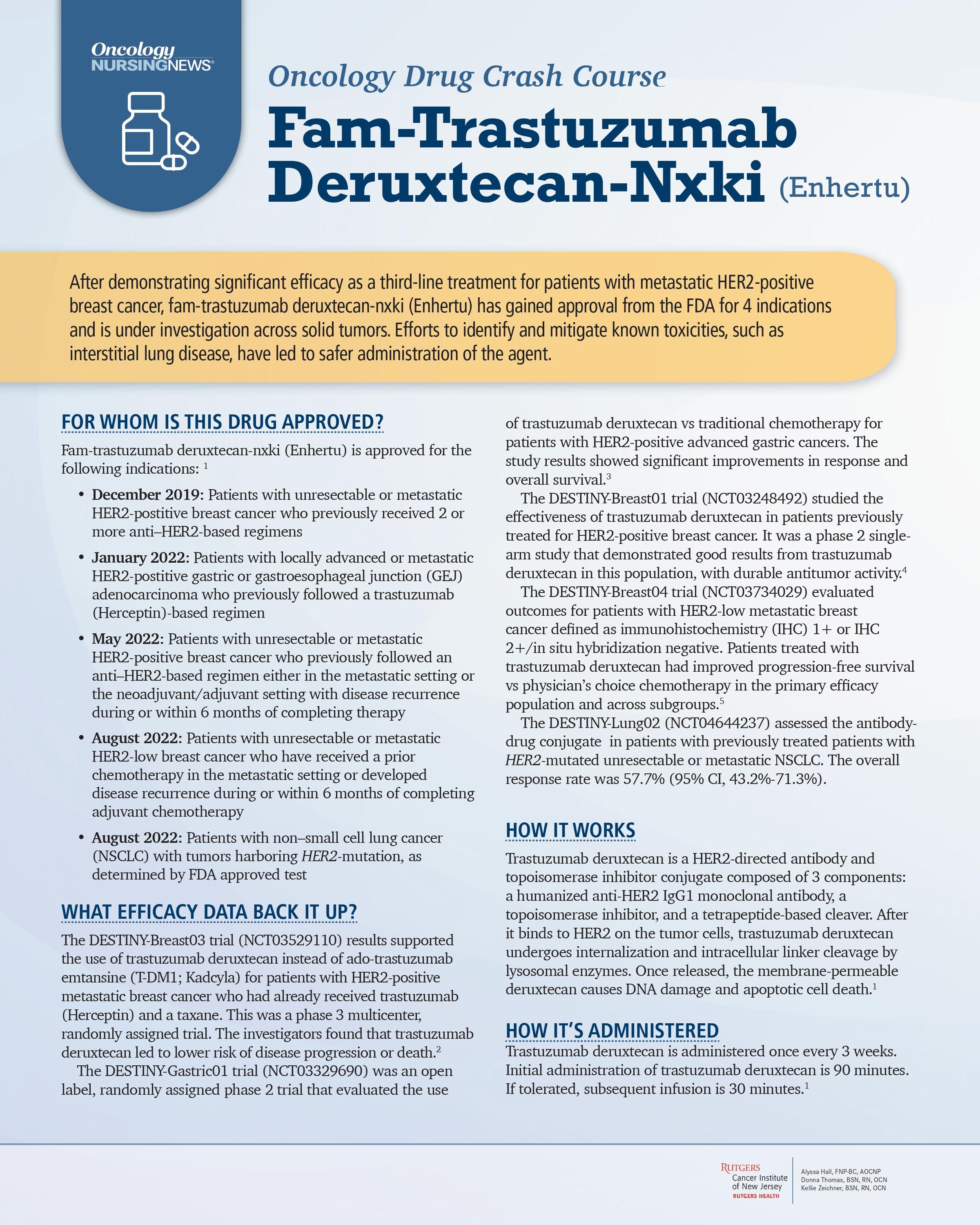
Oncology Drug Crash Course: Fam-Trastuzumab Deruxtecan-Nxki (Enhertu)
After demonstrating significant efficacy as a third-line treatment for patients with metastatic HER2-positive breast cancer, fam-trastuzumab deruxtecan-nxki has gained approval from the FDA for 5 indications and is under investigation across solid tumors.
For a downloadable version that you can print at home, check out our oncology drug crash course page or download here:
FOR WHOM IS THIS DRUG APPROVED?
Fam-trastuzumab deruxtecan-nxki (Enhertu) is approved for the following indications: 1
• December 2019: Patients with unresectable or metastatic HER2-postitive breast cancer who previously received 2 or more anti–HER2-based regimens
• January 2021: Patients with locally advanced or metastatic HER2-postitive gastric or gastroesophageal junction (GEJ) adenocarcinoma who previously followed a trastuzumab (Herceptin)-based regimen
• May 2022: Patients with unresectable or metastatic HER2-positive breast cancer who previously followed an anti–HER2-based regimen either in the metastatic setting or the neoadjuvant/adjuvant setting with disease recurrence during or within 6 months of completing therapy
• August 2022: Patients with unresectable or metastatic HER2-low breast cancer who have received a prior chemotherapy in the metastatic setting or developed disease recurrence during or within 6 months of completing adjuvant chemotherapy
• August 2022: Patients with unresectable or metastatic non–small cell lung cancer (NSCLC) with tumors harboring HER2-mutation, as determined by FDA approved test
WHAT EFFICACY DATA BACK IT UP?
The DESTINY-Breast03 trial (NCT03529110) results supported the use of trastuzumab deruxtecan instead of ado-trastuzumab emtansine (T-DM1; Kadcyla) for patients with HER2-positive metastatic breast cancer who had already received trastuzumab (Herceptin) and a taxane. This was a phase 3 multicenter, randomly assigned trial. The investigators found that trastuzumab deruxtecan led to lower risk of disease progression or death.2
The DESTINY-Gastric01 trial (NCT03329690) was an open label, randomly assigned phase 2 trial that evaluated the use of trastuzumab deruxtecan vs traditional chemotherapy for patients with HER2-positive advanced gastric cancers. The study results showed significant improvements in response and overall survival.3
The DESTINY-Breast01 trial (NCT03248492) studied the effectiveness of trastuzumab deruxtecan in patients previously treated for HER2-positive breast cancer. It was a phase 2 singlearm study that demonstrated good results from trastuzumab deruxtecan in this population, with durable antitumor activity.4
The DESTINY-Breast04 trial (NCT03734029) evaluated outcomes for patients with HER2-low metastatic breast cancer defined as immunohistochemistry (IHC) 1+ or IHC 2+/in situ hybridization negative. Patients treated with trastuzumab deruxtecan had improved progression-free survival vs physician’s choice chemotherapy in the primary efficacy population and across subgroups.
The DESTINY-Lung02 (NCT04644237) assessed the antibodydrug conjugate in patients with previously treated patients with HER2-mutated unresectable or metastatic NSCLC. The overall response rate was 57.7% (95% CI, 43.2%-71.3%).
HOW IT WORKS
Trastuzumab deruxtecan is a HER2-directed antibody and topoisomerase inhibitor conjugate composed of 3 components: a HER2-directed monoclonal antibody, a topoisomerase I inhibitor payload, and a tumor-selective cleavable linker. After it binds to HER2 on the tumor cells, trastuzumab deruxtecan undergoes internalization and intracellular linker cleavage by lysosomal enzymes. Once released, the membrane-permeable deruxtecan causes DNA damage and apoptotic cell death.1
HOW IT’S ADMINISTERED
Trastuzumab deruxtecan is administered once every 3 weeks. Initial administration of trastuzumab deruxtecan is 90 minutes. If tolerated, subsequent infusion is 30 minutes.1
THE RECOMMENDED DOSE
- Breast cancer: 5.4 mg/kg1
- Lung cancer: 5.4 mg/kg
- Gastric cancer: 6.4 mg/kg
HOW TO MANAGE ASSOCIATED ADVERSE EVENTS
Before initial infusion, baseline vital signs, nursing assessment, complete blood count (CBC) results, comprehensive metabolic panel results, pregnancy level, and echocardiogram results must be obtained. CBC is repeated every cycle to monitor for neutropenia, and the echocardiogram is repeated per institutional policy to monitor for left ventricular dysfunction or as clinically indicated.
At Rutgers Cancer Institute of New Jersey in New Brunswick, in addition to physical assessment and patient account, respiratory status is evaluated before each infusion of trastuzumab deruxtecan using a 6-minute walk test with pulse oximetry monitored prior to ambulation and at completion. Safe handling of trastuzumab deruxtecan includes donning 2 pairs of chemotherapy-approved gloves and disposable gown per Oncology Nursing Society guidelines.6
WHAT TO INFORM PATIENTS ABOUT
During initial infusion, patient is instructed to report any acute symptoms of hypersensitivity such as sudden difficulty breathing, facial flushing, itchiness, hives, lower back pain, and chest pain. If a hypersensitivity reaction is noted, trastuzumab deruxtecan administration should be immediately stopped and emergency drugs such as diphenhydramine, famotidine, and dexamethasone administered as per institution policy.
HOW TO SAFELY HANDLE THIS AGENT
Trastuzumab deruxtecan must be protected from light and administered via intravenous line or a central line such as port-a-cath.
HOW TO MANAGE ASSOCIATED ADVERSE EFFECTS
Patients treated in the outpatient setting and their family members should be aware of how to reach their health care team in the event of adverse effects and be taught to go to the emergency department in the event of a life-threatening emergency. Patients receiving trastuzumab deruxtecan should be aware of its most common adverse effects, including nausea, vomiting, fatigue, and alopecia. Nurses should make sure patients have antiemetics readily available at home and know how to take them if needed. Focus of instruction should be on the most serious adverse effects related to trastuzumab deruxtecan, including interstitial lung disease and pneumonitis. Patients should be aware of their baseline respiratory status and understand that if they begin coughing more or develop new or worsening breathing problems, they must reach out to the care team. Also, patients should know cardiac issues can occur with trastuzumab deruxtecan, which is why the health care team will obtain baseline echocardiogram results. However, any new or worsening swelling in the lower extremities, heart palpitations, extreme fatigue, dizziness, and worsening shortness of breath should be reported. Furthermore, patients should be educated on the increased risk for neutropenia with trastuzumab deruxtecan and notify their provider if they develop any symptoms of infection.
References
1. Enhertu. Prescribing information. Daiichi Sankyo Inc; 2022. Accessed July 21, 2022. bit.ly/3vQaR5j
2. Cortés J, Kim SB, Chung WP, et al; DESTINY-Breast03 Trial Investigators. Trastuzumab deruxtecan versus trastuzumab emtansine for breast cancer. N Engl J Med. 2022;386(12):1143-1154. doi:10.1056/nejmoa2115022
3. Shitara K, Bang YJ, Iwasa S, et al; DESTINY-Gastric01 Investigators. Trastuzumab deruxtecan in previously treated HER2-positive gastric cancer. N Engl J Med. 2020;382(25):2419-2430. doi:10.1056/nejmoa2004413
4. Modi S, Saura C, Yamashita T, et al; DESTINY-Breast01 Investigators. Trastuzumab deruxtecan in previously treated HER2-positive breast cancer. N Engl J Med. 2020;382(7):610-621. doi:10.1056/nejmoa1914510
5. Modi S, Jacot W, Yamashita T, et al; DESTINY-Breast04 Trial Investigators. Trastuzumab deruxtecan in previously treated HER2-low advanced breast cancer. N Engl J Med. 2022;387(1):9-20. doi:10.1056/NEJMoa2203690
6. Toolkit for safe handling of hazardous drugs for nurses in oncology. Oncology Nursing Society. 2018. Accessed July 21, 2022. bit. ly/3RRPXw9