High-Touch Wipe Down: Decreasing C. diff Rates in Adults With Cancer
Following a high rate of CDIs, the inpatient medical oncology unit at the University of California, Los Angeles, Santa Monica Medical Center adapted an evidence-based intervention.
Clostridium difficile (C. diff) is a gram-positive, spore-form­ing bacterium noted to be the leading cause of hospi­tal-acquired diarrhea in patients with cancer undergoing chemotherapy.1 A study by Kamboj et al reported C. diff rates to be twice as high in the oncology population compared with all patients in the United States. Oncology patients are at a partic­ularly high risk of C. diff infections (CDIs) due to treatment or disease-related immunosuppression and neutropenia. C. diff is a life-threatening complication for neutropenic patients that can result in septic shock and death.2
The inpatient, 26-bed, medical oncology unit at the University of California, Los Angeles, Santa Monica Medical Center (SMUCLA) had an alarming rate of CDIs. The unit practice coun­cil (UPC) identified the need for environmental disinfection of patient care areas through the adaptation of an evidence-based intervention, high-touch wipe down (HTWD). Due to its sus­tained success in a vulnerable oncology population, HTWD has been implemented hospital wide.
HEALTH SYSTEM C. DIFF PROTOCOL
Within the UCLA health system, C. diff is screened for upon admission and once a shift. A positive screen is indicated by 3 or more loose stools in a 24-hour period. The nursing bun­dle is then activated, prompting staff to place the patient on contact-spore isolation, send a stool sample to rule out C. diff, maintain proper hand hygiene, wear personal protective equip­ment (PPE), and notify the physician. Despite consistently adhering to the organizational policy for early identification of C. diff, CDIs on the oncology unit were above the national median. Our goal was to reduce these rates by 50% from 2014 to October 2015.
PRACTICE CHANGE WITH HTWD
The Centers for Disease Control and Prevention recommends the routine cleaning of environmental surfaces with C. diff sporicidal Environmental Protection Agency—registered disinfec­tant. High-touch surfaces, or those with frequent hand contact, should be cleaned more often than regular housekeeping areas.3 One report revealed a 40.5% decrease in CDIs on a geriatric unit when it was disinfected with bleach versus a neutral detergent.4 A later comparison of 2 intensive care units led to fewer CDIs in both units when adjunct bleach cleaning was performed in all patient rooms and known C. diff rooms alone.
The following HTWD practices were adopted on the SMUCLA oncology unit:
- Store Clorox germicidal bleach wipes in every patient room and at nursing stations.
- Nurses and care partners wipe down high-touch surfaces with bleach wipes once a shift for all patients and twice a shift for neutropenic patients.
- Wipe down all high-touch areas, including the bed frame, call light, doorknobs, countertops, side table, nightstand, monitor cables, and work stations.
- Follow C. diff rates monthly to monitor effectiveness and results.
EMPLOYEE EDUCATION
Baseline staff knowledge of C. diff prevention was assessed with a pre-survey, followed by a tailored education plan and a subsequent post survey. The outcome was an overall improvement of staff understanding of HTWD. Employees were edu­cated with informational flyers and a PowerPoint presentation during huddles, staff meetings, and annual skills labs.
DECREASING C. DIFF RATES
HTWD was initiated on the oncology unit in February 2015. The rate of CDIs per 10,000 patient days (PDs) decreased from 14.99 in 2014 to zero from February to July 2015. We exceeded our goal of a 50% reduction when comparing C. diff rates from 2014 to recent years. In 2016, just 6.1 cases per 10,000 PDs were reported, and the most current data from 2017 shows a further decrease to 3.4 cases per 10,000 PDs. The HTWD is simple and inexpen­sive but can be highly effective (Figures 1 and 2).
CAPTION
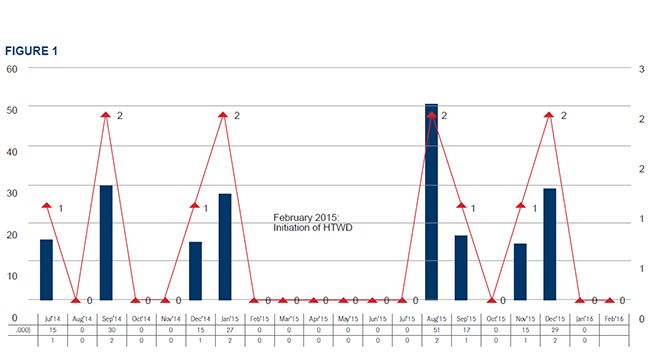
FIGURE 1. Oncology Unit C. diff Rates: July 2014-February 2016
Note: 2014 baseline CDIs = 14.99 per 10,000 PDs. HTWD implemented February 2015 with no CDIs for 6 months. Blue bar is incidence per 10,000 PDs. Red line is number of cases.
C. diff indicates Clostridium difficile; CDI, C. diff infections; HTWD, high-touch wipe down; PD, patient day.
CAPTION
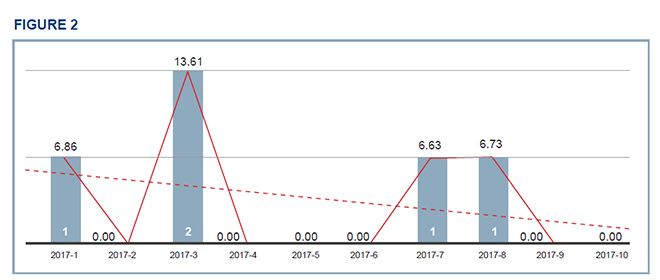
FIGURE 2. Oncology Unit C. diff Rates: January 2017-October 2017
Note: 2017 most recent C. diff rates = 3.4 per 10,000 PDs. Significant reduction compared with baseline. Blue bar is number of cases. Red line is incidence per 10,000 PDs.
C. diff indicates Clostridium difficile; PD, patient day.
ADDRESSING BARRIERS
Several barriers were identified upon adding HTWD to unit workflow. Oncology patients endorsed sensitivity to the smell of bleach, exacerbating symptoms such as nausea and diz­ziness. By offering aromatherapy or encourag­ing ambulation during HTWDs, patients were agreeable to using bleach wipes and eager to have HTWDs completed.
Feedback from staff included problems with skin irritation and uniform staining. The Association for Professionals in Infection Control and Epidemiology suggests the use of PPE when cleaning with bleach.5 Wearing masks, gowns, and gloves has been an effective solution for employee protection.
Finally, the lack of formal HTWD documentation posed a great challenge. Ongoing discussions to integrate HTWD into the electronic record ended due to concerns surrounding scope of practice. Oncology staff recognize the importance of HTWD in protecting our patients and currently document completion on paper.
MOVING FORWARD
The success of the HTWD was recognized by the chief nursing officer and transformational lead­ership shared-governance Magnet council as a nursing best practice and key strategy for fiscal year 2017-2018. SMUCLA implemented HTWD in February 2017 after extensive interprofes­sional collaboration and planning with stake­holders. UPCs and unit leadership provided stan­dardized education materials, campaign flyers, and hands-on training for staff. C. diff rates will continue to be evaluated over time as HTWD is applied to the broad patient population within the organization.
IMPLICATIONS FOR PRACTICE
Performing HTWD as part of a bundle dramati­cally reduced C. diff rates on a medical oncology unit. CDIs were eliminated for 6 months follow­ing the project’s initiation, during which time intensive education and daily reminders were given. Ramphal, Suzuki, McCracken, and Addai demonstrated a 60% increase in compliance with HTWDs through repeated training.6 As evidenced by fluctuating C. diff rates, continued education, peer-to-peer accountability, and a follow-up tool are essential to the sustainability of this practice. The oncology unit will begin a trial using ultravi­olet light audits next year to evaluate consistency and compliance.
New 2017 Joint Commission and CMS guide­lines have brought nosocomial CDIs to the fore­front of nursing quality indicators. Incorporating nurse-driven environmental cleaning into hospi­tal-based infection control practices may provide the comprehensive program needed to decrease C. diff rates and improve patient outcomes in the acute care setting.
References
1. Kamboj M, Son C, Cantu S, et al. Hospital-onset Clostridium difficile infection rates in persons with cancer or hematopoietic stem cell transplant: a C3IC network report. Infection Control Hosp Epidemiol. 2012;33(11):1162-1165. doi: 10.1086/668023.
2. Fuereder T, Koni D, Gleiss A, et al. Risk factors for Clostridium difficile infection in hemato-oncological patients: a case control study in 144 patients. Sci Rep. 2016;6:31498. doi: 10.1038/srep31498.
3. Centers for Disease Control and Prevention. Guidelines for environmental infection control in health-care facilities (2003). CDC website. cdc.gov/infectioncontrol/guidelines/environmental/background/services.html#. Updated November 5, 2015. December 10, 2017.
4. MacLeod-Glover N, Sadowski C. Efficacy of cleaning products for C. difficile: environmental strategies to reduce the spread of Clostridium difficile-associated diarrhea in geriatric rehabilitation. Can Fam Physician. 2010;56(5):417-423.
5. Association for Professionals in Infection Control and Epidemiology. Guide to preventing Clostridium difficile infections. APIC website. apic.org/Resource_/EliminationGuideForm/59397fc6-3f90-43d1-9325-e8be75d86888/File/2013CDiffFinal.pdf. Published 2013. Accessed December 10, 2017.
6. Ramphal L, Suzuki S, McCracken IM, Addai A. Improving hospital staff compliance with environmental cleaning behavior. Proc (Bayl Univ Med Cent). 2014;27(2):88-91.

Nursing Perspectives on Managing Toxicities With ADCs in Metastatic Gastric and Breast Cancers
September 1st 2022In this episode of "The Vitals," Sarah Donahue, MPH, NP, AOCNP; Jamie Carroll, APRN, CNP, MSN; Theresa Wicklin Gillespie, PhD, MA, RN, FAAN; and Elizabeth Prechtel-Dunphy, DNP, RN, ANP-BC, AOCN, exchange clinical pearls for treating patients receiving antibody-drug conjugates.
Innovative Program Reduces Nurse Turnover and Fosters Development
Published: September 12th 2024 | Updated: September 12th 2024The US Oncology Network (The Network) has developed one of the most comprehensive programs in the nation to support the professional development and retention of new oncology nurses.



