- September 2011
- Volume 5
- Issue 5
Cancer Screening: Are You Recommending the Right Intervals?
Now more than ever, oncology nurses need to be able to fill the knowledge gap and accurately educate their patients and the public about cancer screening tests and their frequency.
Now more than ever, oncology nurses need to be able to fill the knowledge gap and accurately educate their patients and the public about cancer screening tests and their frequency.
The news media has done a good job of informing the public about cancer screening. So good, in fact, that it seems that not a day goes by without hearing that one organization or another has issued updated guidelines and recommendations. As oncology nurses, we’re expected to be knowledgeable about cancer screening. Our patients, the public, and even our own health depend on our having an accurate and up-to-date knowledge base.
Let’s start with mammograms. In July 2011, the American College of Obstetricians and Gynecologists (ACOG) issued new breast cancer screening guidelines that recommend that women begin having screening mammograms annually at age 40. Previous ACOG guidelines recommended mammograms every 1 to 2 years starting at age 40 and annually beginning at age 50. ACOG cited the incidence of breast cancer, the sojourn time for breast cancer growth, and the potential to reduce the number of deaths from breast cancer as the rationale for revising their breast cancer screening guidelines.1
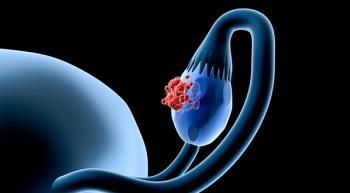
Now on to cervical cancer screening. Current cervical cancer screening guidelines, issued by the American Cancer Society (ACS) in June 2011 and ACOG in November 2009, recommend a combination of a Papanicolaou (Pap) test and a human papillomavirus (HPV) test for women age 30 and older. Upon screening, if the results of these 2 tests are normal, women can wait 3 years for their next cervical cancer screening test.2,3
In June 2011, researchers from Kaiser Permanente in northern California reported that their National Cancer Institute—initiated study of 33,818 women in community settings supports the ACS and ACOG recommendation. They concluded that concurrent Pap test and HPV testing allowed the screening interval to be safely extended to 3 years for women who had negative HPV tests and normal Pap smears.4
Despite the evidence and recommendations from well-respected and reputable organizations, there’s been reluctance to implement a 3-year cervical cancer screening interval recommendation in clinical practice. Researchers from the Centers for Disease Control and Prevention (CDC) recently found that primary care providers still recommend annual cervical cancer screening. According to the study, <15% of the 592 physicians surveyed extend the screening interval when using the Pap and HPV tests together, as the ACS and ACOG guidelines recommend. The CDC analysis found that there is a need for healthcare provider education, and noted that use of Pap and HPV testing and adherence to the extended screening interval reduces patient harm caused by overtesting, such as pain, inconvenience, morbidity, and unnecessary followup procedures and treatments. The CDC researchers also identified the need for continued surveillance on cervical cancer screening guideline adherence.5
Obviously, adhering to cancer screening interval guidelines requires awareness and knowledge of the currently recommended guidelines. As oncology nurses, we need to stay abreast of cancer screening guidelines and counsel our patients appropriately. For many women, lowering the age at which breast cancer screening should begin makes perfect sense. However, increasing the interval of cervical cancer screening from annually to every 3 years is not as easily understood. After all, even physicians are grappling with the new interval recommendation. Now more than ever, oncology nurses need to be able to fill the knowledge gap and accurately educate their patients and the public about cancer screening tests and their frequency.
Lisa Schulmeister, RN, MN, APRN-BC, OCN®, FAAN, is an oncology nursing consultant and adjunct assistant professor of nursing at Louisiana State Health Sciences Center in New Orleans, LA, and the editor-in-chief of OncLive Nursing.
References
- American College of Obstetricians and Gynecologists. Annual mammograms now recommended for women beginning at age 40. http://bit.ly/ pZs5xs. Accessed August 20, 2011.
- American Cancer Society. Cervical Cancer: Prevention and Early Detection. http://bit.ly/nBKLNz. Accessed August 20, 2011.
- American College of Obstetricians and Gynecologists. ACOG Practice Bulletin no.109: cervical cytology screening. Obstet Gynecol. 2009;114(6):1409-1420.
- Katki HA, Kinney WK, Fetterman B, et al. Cervical cancer risk for 330,000 women undergoing concurrent HPV testing and cervical cytology in routine clinical practice. In: J Clin Oncol 29 (15 suppl). Chicago, IL: American Society of Clinical Oncology; 2011. Abstract 1508.
- Roland KB, Soman A, Benard VB, et al. Human papillomavirus and Papanicolaou tests screening interval recommendations in the United States [published online ahead of print June 12, 2011]. Am J Obstet Gynecol. doi:10.1016/j.ajog.2011.06.001.
Articles in this issue
over 14 years ago
Case Presentation: Myelodysplastic Syndromesover 14 years ago
Living With Multiple Myeloma: Nurses as the Lifelineover 14 years ago
Compassion Fatigue: When Caring Takes Its Tollover 14 years ago
The Caring Ambassadors Programover 14 years ago
Noninvasive Stool Test Effectively Detects Colon CancerNewsletter
Knowledge is power. Don’t miss the most recent breakthroughs in cancer care.