Advancing Multiple Myeloma Treatment With CAR T-Cell Therapy
Daniel Verina, DNP, ACNP-BC, discussed how CAR T-cell therapy is changing the treatment landscape for patients with multiple myeloma.
Advancing Multiple Myeloma Treatment With CAR T-Cell Therapy
CAR T-cell therapy represents a significant advancement in the treatment of multiple myeloma, especially as its ability to provide deep and durable responses offers renewed hope to patients and healthcare providers alike, an expert said.
During a Community Case Forum event focused on the use of CAR T-cell therapies for the treatment of multiple myeloma, Daniel Verina, DNP, ACNP-BC, nurse practitioner at The Mount Sinai Hospital in New York, New York, discussed the evolution of the treatment landscape for this disease.
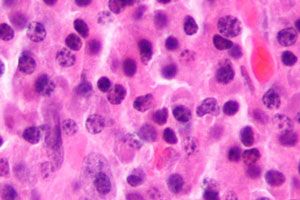
The field of multiple myeloma treatment is experiencing a renaissance with the advent of novel therapies, particularly CAR T-cell therapy. This groundbreaking approach is reshaping patient outcomes and offering hope where conventional treatments have fallen short. One of the most promising CAR T-cell therapies in this domain is ciltacabtagene autoleucel (Carvykti; cilta-cel), which has demonstrated remarkable efficacy and durability in treating this challenging disease.
Understanding CAR T-Cell Therapy
CAR T-cell therapy involves modifying a patient's T-cells to express a chimeric antigen receptor (CAR) that specifically targets and destroys cancer cells. Unlike traditional treatments, CAR T-cell therapy leverages the body's immune system to fight cancer more effectively. "We're using a different type of T cell," explains Verina. "Now we're re-engineering a T cell to go after the patient's own myeloma".
Efficacy and Patient Outcomes
The efficacy of cilta-cel, a BCMA-directed CAR T-cell therapy, has been a game-changer for patients with multiple myeloma. In clinical trials, cilta-cel has shown impressive response rates and prolonged progression-free survival (PFS). Verina notes, "at 18 months, 41% of the patients still had a good progression-free survival." This is a significant improvement compared to standard therapies, where PFS is typically much shorter.
Moreover, the depth of response achieved with cilta-cel is noteworthy. Approximately 71% of patients treated with this therapy achieved an overall response, with 35% reaching minimal residual disease (MRD) negativity. "That's rare for us in myeloma because we're always about more therapies, more than one therapy at the same time," Verina emphasizes.
Integrating Cilta-cel into Treatment Plans
Cilta-cel is now an integral part of the treatment landscape for multiple myeloma, particularly for patients who have exhausted other options. The approval of cilta-cel has expanded the arsenal of available therapies, providing new hope for patients. For example, idecabtagene vicleucel (ide-cel; Abecma) was approved by the FDA in March 2021 for the treatment of patients with relapsed/refractory multiple myeloma after receiving 4 or more lines of prior therapy. Then in March 2022, cilta-cel received FDA approval for that same indication. The FDA then approved cilta-cel for the treatment of relapsed/refractory multiple myeloma who had previously received 1 line of therapy.
The treatment process for CAR T-cell therapy involves several steps, including T-cell collection, modification, and reinfusion. While the manufacturing process can take several weeks, the wait is often justified by its benefits. "The collection is simple for a patient per se, but it has to be manufactured here. It does take 2 to 4 weeks. But we have seen manufacturing take up to 6 to 8 weeks to get certain cells back," Verina explains. “So it is a longer period of time than a 3-day harvest for a stem cell [transplant].”
Addressing Challenges and Side Effects
Despite its promise, CAR T-cell therapy is not without challenges. One significant concern is the potential for side effects, including cytokine release syndrome (CRS) and neurotoxicity. However, the safety profile of cilta-cel has been manageable, with most CRS cases being mild to moderate.
Moreover, the risk of secondary malignancies has been flagged with CAR T-cell therapies, necessitating vigilant monitoring. "We do have to talk about the black box warning that came out with both of these [regarding] secondary malignancies," Verina emphasizes, stressing the importance of transparency and patient education regarding potential risks.
Future Directions and Hope
The future of CAR T-cell therapy in multiple myeloma looks promising, with ongoing research aimed at improving its efficacy and safety. As Verina aptly puts it, "It's the renaissance … where we’re rebirthing. We have new therapies coming out every day. And really what we’re trying to figure out is what are these therapies and where do they fit in our patients’ journey, and even as healthcare providers, how do we make decisions.”
The continuous evolution of CAR T-cell therapy and its integration with other treatments holds great potential for enhancing patient outcomes and extending survival.



