Study Finds Mouth Rinse Alleviates Oral Mucositis Symptoms in Head and Neck Cancers
A growing understanding of the biological pathways at work in the development of oral mucositis in patients treated with cytotoxic cancer therapies has helped spur interest in steering symptom management away from "institutional folklore" rinses and anecdotal approaches toward evidence-based strategies
Stephen T. Sonis, DMD, DMSc
A growing understanding of the biological pathways at work in the development of oral mucositis in patients treated with cytotoxic cancer therapies has helped spur interest in steering symptom management away from “institutional folklore” rinses and anecdotal approaches toward evidence-based strategies, according to a leading expert about the toxicity.
Against this backdrop, Access Pharmaceuticals Inc launched a multicenter, randomized, blinded clinical trial among patients with head and neck cancers to evaluate its mucoadhesive hydrogel (MuGard) oral wound rinse against a control rinse, although the Dallas-based company had no regulatory requirement to do so, noted Stephen T. Sonis, DMD, DMSc, who designed the study.
The study found that patients who rinsed with MuGard on the first through last day of their radiation therapy reported less mouth and throat soreness (MTS), a delayed onset of significant MTS, and lower usage of opioids than those who used a control “standard of care” rinse.1
“The patients who used MuGard had statistically less discomfort measured by area under the curve [AUC] of this outcome versus patients who received placebo,” said Sonis in an interview.
Mucositis Has Significant Impact
Oral mucositis represents a significant area of unmet need for patients with cancer, said Sonis, who specializes in the treatment of oral soft tissue disease at the Dana-Farber Cancer Institute and Brigham and Women’s Hospital in Boston, Massachusetts.
Overall, approximately 8% of all newly diagnosed patients with cancer are at a high risk (>50% chance) of developing ulcerative mucositis, while between 20% and 49% of patients face an intermediate risk of the toxicity sometime during the course of their treatment.2 Ultimately, about 450,000 patients will develop clinically significant oral mucositis this year in the United States.
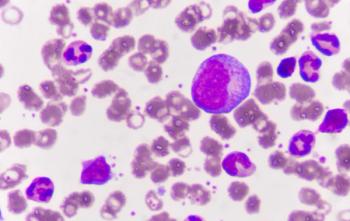
The incidence of oral mucositis approaches 80% of patients with head and neck cancers and about 40% of individuals who have undergone hematopoietic stem cell transplant (HSCT), and also is prevalent in patients with breast, colorectal, and lung cancers.
“If you ask patients who’ve had ablative chemotherapy or patients who’ve had radiation to the head and neck to rank side effects of their treatment, mucositis is consistently at the top of the list,” said Sonis. “It causes enormous amounts of pain.”
Outcomes and healthcare costs also are affected, as patients may limit therapy or require other medications or even hospitalization due to mucositis-associated problems; incremental costs among individuals treated for cancers of the lung and head and neck were estimated at approximately $18,000 per patient.1
Changing Treatment Landscape
Despite the prevalence of oral mucositis, treatment options are limited and are typically not based on clinical trial evidence, said Sonis.
In fact, he noted, most of the products used to alleviate oral mucositis symptoms gained marketing approvals under the FDA’s medical devices program, which involves a less rigorous standard than a new drug would undergo. Some centers use rinses developed informally, such as “magic mouthwash” or “miracle mouthwash.”
“They’re formulations based on institutional folklore so they vary from place to place,” said Sonis. “They’re used to palliate patients—usually not that effectively.”
Palifermin (Kepivance), a human keratinocyte growth factor, is the only agent that the FDA has specifically approved for oral mucositis, according to Sonis. The agent, approved in 2004, is indicated for intravenous administration in patients with hematologic malignancies who are undergoing HSCT after myelotoxic therapy.
Interest in developing therapies for oral mucositis is growing now that the mechanisms that lead to the toxicity are better understood, said Sonis. Historically, researchers believed that oral mucositis and stomatitis result from a breakdown in the natural process of epithelium renewal during cytotoxic cancer therapy.
“The historical idea was that if you gave radiation or chemotherapy, the agent simply couldn’t differentiate between rapidly dividing normal cells and rapidly dividing cancer cells, and so the normal cells were indiscriminately killed, the renewal didn’t take place, the tissue broke down and was ulcerated,” said Sonis. “It sounds like a very straightforward paradigm, and it is, but it’s not true. There’s much more biology involved, many more pathways involved than were originally realized.”
Key Findings in MuGard Study
MuGard is a viscous liquid nanopolymer formulation that forms a protective coating over the oral mucosa. In 2006, the FDA approved the rinse under its 510(k) medical devices program with indications for the management of oral mucositis or stomatitis caused by radiation or chemotherapy and for other types of oral mouth wounds such as canker sores and ulcers from surgery, dentures, or braces.
For the study, 120 patients were randomized to use either MuGard or a flavored saline bicarbonate rinse; 78 patients who documented that they used the rinse during the first 2.5 weeks of radiation therapy were included in the results.
More than 90% of those 78 patients had cancers of the oral cavity or the oropharynx as their primary tumor site, including approximately 70% with stage IVA/B disease, and were scheduled to receive a median cumulative radiation dose of 70 Gy.
Participants were asked to rinse with 5 mL of mouthwash for a full minute, with a goal of four times a day, starting on the first day of radiation therapy and continuing until the last day.
The primary endpoint was a reduction in MTS defined by AUC as reported by the patient as part of the Oral Mucositis Daily Questionnaire (OMDQ), with a P value <.05 considered statistically significant.
Secondary endpoints included the use of opioids, which were among the supportive therapy agents that investigators could provide under the study protocol, and other measures of healthcare resource use.
Among the 37 patients who rinsed with MuGard, the mean AUC was 68.0 versus 86.1 for the 41 patients who used the control rinse, for a statistically significant advantage (P = .034).
In addition, patients in the MuGard group experienced a longer time to first occurrence compared with the control arm (28 days vs 19 days) and were less likely to receive opioid analgesia (70% vs 76%). Patients who used MuGard also lost less weight, although these advantages were not statistically significant.
References
- Allison RR, Ambrad AA, Arshoun Y, et al. Multi-institutional, randomized, double-blind, placebo-controlled trial to assess the efficacy of a mucoadhesive hydrogel (MuGard) in mitigating oral mucositis symptoms in patients being treated with chemoradiation therapy for cancers of the head and neck. Cancer. 2014;120(9):1433-1440.
- Sonis ST. Mucositis: the impact, biology and therapeutic opportunities of oral mucositis [published online October 13, 2009]. Oral Oncol. 2009;45(12):1015-1020.
Newsletter
Knowledge is power. Don’t miss the most recent breakthroughs in cancer care.