New Strategies Provide Faster Access To Cancer Care For Patients
Pilot programs based out of Yale Cancer Center and Moffitt Cancer Center seek to improve access for newly diagnosed patients with cancer.
Sarah Mougalian, MD

Addressing access to care is the first steps to improving patient outcomes, according to investigators with Yale Cancer Center and Moffitt Cancer Center. Ensuring that patients reach the right providers at the right team is key in being able to provide potentially life-saving agents and personalized treatments.
“Access is a multifaceted construct. It’s not just about the onboarding process or the amount of time that it takes to get that first appointment. It also ensures that the patient can reach a live person when they make a phone call, that they can be seen in a convenient location be seen by a clinician who is an expert in their specific disease, that they [can] access information about their diagnosis that’s readily available, and be able to afford their care,” Sarah Mougalian, MD, said during the 2022 National Comprehensive Cancer Network (NCCN) Annual Conference.1 She added that treatment should not only be prompt, but also have seamless transitions from the first appointment through every phase of the cancer care continuum. Mougalian is chief ambulatory officer at Yale Cancer Center/ Smilow Cancer Hospital and an associate professor of medicine in medical oncology at Yale School of Medicine in New Haven, Connecticut.
Sustainable care following the first point of contact the management of logistics of care affects both the patient and the provider. “The moment that one has a diagnosis [of cancer], they are overcome with a sense of fear and urgency,” Christie Pratt, MA, DHSc, said on a panel at the 2022 NCCN Annual Conference. “At that moment both patients and their loved ones need help. It’s about more than just getting them to the best care. It’s deeper than that,” Pratt is the senior director of Moffitt Medical Group at Moffitt Cancer Center in Tampa, Florida.
Data from a recent meta-analysis of mortality rates across the most common cancer types— bladder, breast, colon, rectum, lung, cervix, and head and neck—demonstrated that delays in cancer treatment initiation were associated with increased risk of death if delayed by 4 weeks or more.2 For example, a 13% increased risk of death was associated with a 4-week delay in adjuvant systemic treatment for patients with colorectal cancer.2 Hazard ratios for delays in systemic treatments had singificant associations with delays of 4 weeks in neoadjuvant treatment of bladder cancer (HR, 1.24; 95% CI, 1.03-1.50), adjuvant treatment of breast cancer (HR, 1.09; 95% CI, 1.07-1.11). Additionally, radiotherapy delays in head and neck cancer (HR, 1.09; 95% CI, 1.05-1.14) and cervical cancer (HR, 1.23; 95% CI, 1.00-1.50) were deemed significant.2
Investigators cited patient, disease, and system factors all play a role in delays to care, the most cited reasons being workups and specialist consultations. To alleviate the burden of even one of these factors could significantly improve delays in treatment.2
Mougalian and Pratt presented 2 initiatives to improve new patient access to cancer care at Yale Cancer Center/Smilow Cancer Hospital and Moffit Cancer Center, respectively.1 The programs focused on systemic hurdles, namely reducing delays for patient appointments with disease specialists.
Waiting is the Worst Part
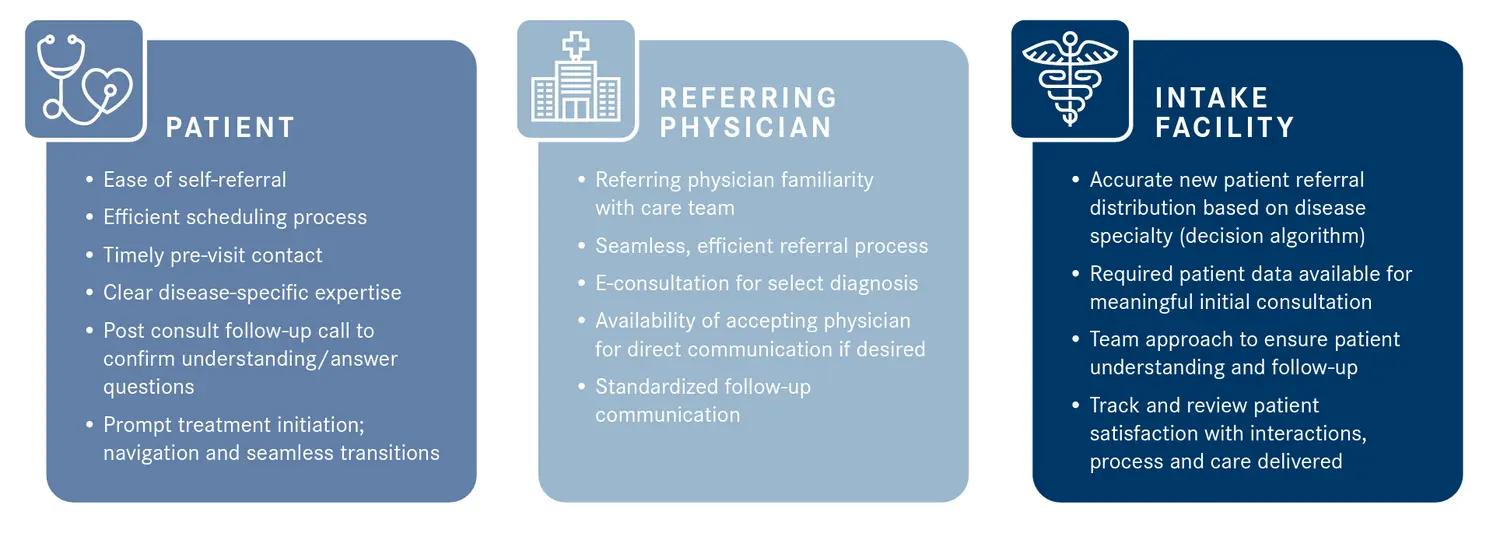
Developing a system with a patient-centric focus, investigators at Yale Cancer Center initiated a pilot program to offer patients next day access to care following a diagnosis of cancer. Mougalian and her colleagues began with 2 subspecialty clinics at the institution—breast and gynecologic oncology. “We want it to be easy [for the patient following their] initial consultation to self-refer [and] for the scheduling process to be efficient,” Mougalian said. “We want the patient to be able to see a provider who is expert in their diagnosis in a timely fashion or institutional goal is within 5 days. Both before and after the first appointment, the patient should be able to speak with someone knowledgeable in the process and understanding of the plan of care.”
Investigators in the breast and gynecologic clinics were tasked with developing individual implementation plans that included an algorithm to define which patients were eligible for next day access (Figure 11). Selected patients typically included those who had received a diagnosis of cancer or suggestion of cancer prior to referral. The institutional goal of the pilot program was to have patients obtain appointments within 5 days. Early findings of the program were presented at the 2021 American Society of Clinical Oncology Quality Care Symposium.3
Figure 1. The Ideal State of Patient-Centric Access to Care1
The analysis included 3107 new patients who had a referral meeting across 4 sites of the institution. The primary efficacy measures of the program were to evaluate the number of patients who were seen within 1 business day of their referral, time to their first visit, the number of patients who accepted a next day appointment, and to obtain a descriptive analysis of the reasons why a next day appointment was not taken. Among the entire population of patients seen, 900 were eligible for next day visits with 12% of patients accepting the appointment. More patients with breast cancer (17%) accepted next day visits than those who received a diagnosis of gynecologic cancer (9%).3
The median time to first visit was measured at 2 time points: December 2019 through February 2020, and December 2020 through February 2021. The median time to next visit in the first year was 13 days vs 9 days in the second year.3
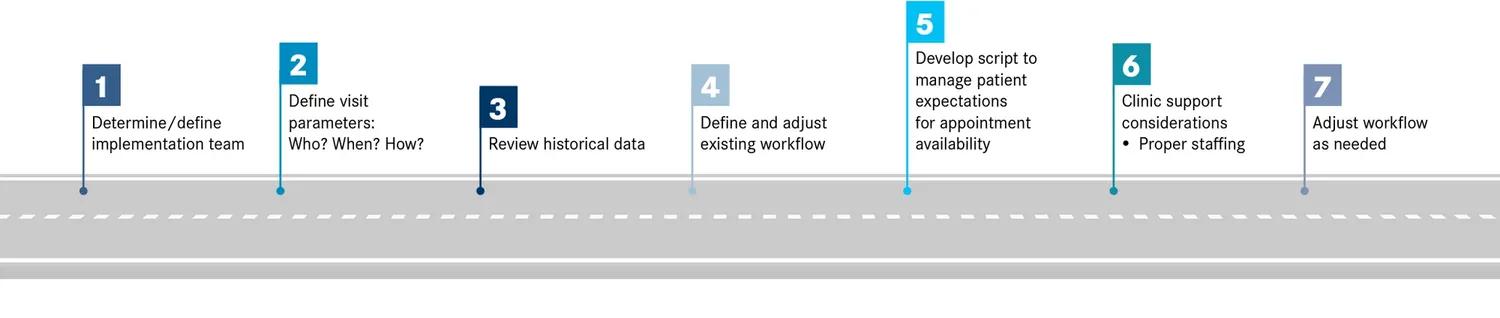
Mougalian stressed the importance of care team coordination through the process. “For providers who refer to us, the process should also be seamless and efficient,” she said. “Appointments should be scheduled quickly and follow-up and notes from the first consultation should be relayed back to the referring physician.” Mougalian added that special attention should also be paid to internal staffing challenges with even distribution of patient cases among appropriate specialists within the disease state. “Each team reviewed historical data to estimate the volume of new patient slots [and] made the appropriate adjustments in scheduling,” she said.1
In contrast with their internal goal, investigators also strived to meet patient where they were. “The patient was at the center of this initiative and the No. 1 goal was to honor the patient’s choice, offering an appointment as soon as the patient wants it, and where the patient prefers,” Mougalian said. In tandem with this, she noted that managing patient expectations was also a critical component of the process, including the limitations that come with a next day appointment and other options that were available to them. An example roadmap for implementation is outlined in Figure 2.1
Figure 2. Roadmap to Implementation and Maintaining Patient Access1
In an analysis of patients with a data cutoff of February 2021, reasons why patients did not accept a next day appointment included the availability of a specific provider (49%) or a specific date was requested (27%). These rates dropped in an analysis between August 2021 and January 2022 to 38% and 20%, respectively.
Overall patients were satisfied with their scheduling through the next day access program with 92% of respondents (n = 864) stating that they were satisfied with their appointment choices. Further, 67% said the appointments exceeded their expectations with 29% stating that the appointment met their expectations. “We also asked on a scale of 1 to 10: How would you rate your first visit? The average was 9.4, and the median was 10 [ range, 4-10],” Mougalian said.
Oncologist feedback was also collected during the process with some providers noting that the appointments often felt inefficient and harder to navigate, especially if they did not have a comprehensive snapshot of the patient’s records for clinical review. “In general, the feedback was positive, and it was [noted] that patient satisfaction [as well as] excellent responses from providers who referred [patients] was a market differentiator and was going to drive referrals going forward,” Mougalian said.
Patient-First Focus
At Moffit Cancer Center, a similar program, First Connect, was initiated to establish care expectations for patients, enhance multidimensional approaches to care including access to clinical trials and personalized medicine, and improve access to visits with a 1-day turnaround from intake to appointment with a clinical subject matter expert.1 “The goal of First Connect was to not only create and provide patients with access, but [execute] it in a very meaningful way,” Pratt said.
The First Connect program starts with a call during which 3 main components are tackled: clinical assessment to support additional work-up requests and initiate a suspected clinical pathway; accelerate access to care by aligning the right provider with the right patient; and to build a foundational component with the patient. A key differentiator of the construct of the Moffit Cancer Center program is an increased focus on the emotional bond with the patient to help alleviate anxiety and build connections with the clinical team, Pratt said.
“The First Connect call is scheduled 24 hours after a patient has entered into our system,” Pratt said. “These calls are prior to a destination visit and serve as the connection that that patient can make with the clinic [and with] a provider who has the knowledge base about the disease can help set expectations. The most important piece is that the patient feels comfortable, understands, and is prepared for the destination visit.” In addition to establishing that connection, Pratt noted that these calls are aimed at patient retention. “Approximately 12% of patients who call into our system, get put into a queue to be scheduled, and then we lose them, they never complete a new patient appointment,” Pratt said. “And that could be because they cancelled the appointment or because we were unable to ever get a hold of them, or that they [were a no show]. We really wanted this to be a way to make that connection and let the patient know, we care, we want to begin the process, and start collecting records to show you that we’re invested in your care and getting you to that consulate visit to start the journey.”
An important component of the pilot program is also generating an increased awareness of the institution’s offerings. “We want to make sure that we market to providers, so that if you’re [a clinician] who’s messaging to your patients is that their cancer diagnosis is your top priority, we now offer the opportunity to speak to a cancer expert within 1 day,” Timothy A. Price, MBA, FACHE, director of patient access at Moffitt Cancer Center said.
Overcoming Barriers to Implementation and Care
Operational and cultural barriers present hurdles for both referring physicians and institutional teams to overcome. Multilevel problems are affecting diversity in clinical trial enrollment from a patient, health system, provider, and community aspect. Should the pilot programs reach the community in their intended ways, increased engagement between providers and referring clinicians may open the door for improved institutional infrastructure across sites to promote enrollment and recruitment. Although the changes may be minimal at this level, these programs afford the treating institutions data sets they did not previously have access to.
“These [programs are] important for the organization because they become a very rich data set,” Price said. “Really understanding patient preference and what’s actually happening with our scheduling data, [we can] harness the power [and] leverage that information for modality planning and looking at our clinical pathways for developing better clinical trial matching.”
Both Price and Mougalian drew attention to turnover and staffing issues which may affect the consistency of these programs to meet their objectives. “We saw that the number of available slots declined over time to and that we largely attribute to faculty departures,” Mougalian said.
“For us, from a [registered nurse] RN perspective, across the nation we have nursing challenges,” Price said. “They have clinical responsibilities [so we must] monitor to see if it is still appropriate delegation of responsibilities knowing some of the constraints that the departments. We wanted to call this out because post pandemic we have seen a rise in calls. How do we deal with those volumes?” One avenue Price noted is maintaining the high-quality call and providing training to get the most out of the interaction and establish that meaningful connection.
“We really need to be thinking about the capacity and the scalability of this,” Price said. “We need to take a look at how they manage their clinical duties and making sure that they’re getting credit for the work that they’re doing.”
Mougalian agreed noting that the minimum data that a patient and the referred physician receive prior to the first appointment should be meaningful. “The team should work together to ensure that the patient understands the plan of care that follow-up is established and that the patient is satisfied with the interactions, the process, and the care that’s delivered,” she said.
“There is no silver bullet for access,” Price said. “We really need to be doing things that have an upstream effect and [can change] the system.”
References
- Mougalian S, Pratt C, Price TA. Strategies and initiatives to improve new patient access to cancer care. Presented at: 2022 National Comprehensive Cancer Network Annual Conference. March 30-April 2, 2022; Accessed May 3, 2022. bit.ly/3wj3RgH
- Hanna TP, King WD, Thibodeau S, et al. Mortality due to cancer treatment delay: systematic review and meta-analysis. BMJ. 2020;371:m4087. doi:10.1136/bmj.m4087
- Mougalian SS, Shomsky L, Campos MM, Chiang AC. “The waiting is the worst”: development of a next day access (NDA) program for patients with cancer. J Clin Oncol. 2021;39(suppl 28):205. doi:10.1200/JCO.2020.39.28_suppl.205
This article was originally published on OncLive® as “New Programs Unlock Patient Access to Oncology Care.”


