Managing Adverse Effects of CAR T-Cell Therapy in Multiple Myeloma
Donna Catamero, ANP-BC, OCN, CCRC, discusses the importance of quickly identifying and managing adverse effects from CAR T-cell therapy in patients with multiple myeloma.
Managing Adverse Effects of CAR T-Cell Therapy in Multiple Myeloma
As CAR T-cell therapy continues to revolutionize the treatment of patients with multiple myeloma, oncology nurses play a vital role in managing the adverse effects associated with this therapy, highlighting the importance of early detection, prompt intervention, patient education, and interdisciplinary collaboration, an expert said.
Donna Catamero, ANP-BC, OCN, CCRC, associate director of the Multiple Myeloma Research Program at The Mount Sinai Health System in New York, New York, discussed the use of CAR T-cell therapy to treat patients with multiple myeloma.
The treatment landscape for multiple myeloma has seen significant advancements with the introduction of CAR T-cell therapy. This innovative approach offers new hope for patients with relapsed or refractory multiple myeloma.
However, the complex nature of CAR T-cell therapy comes with its own set of challenges, especially regarding the management of adverse effects. Oncology nurses play a pivotal role in ensuring the safety and well-being of patients undergoing this treatment.
Understanding CAR T-Cell Therapy and Its Adverse Effects
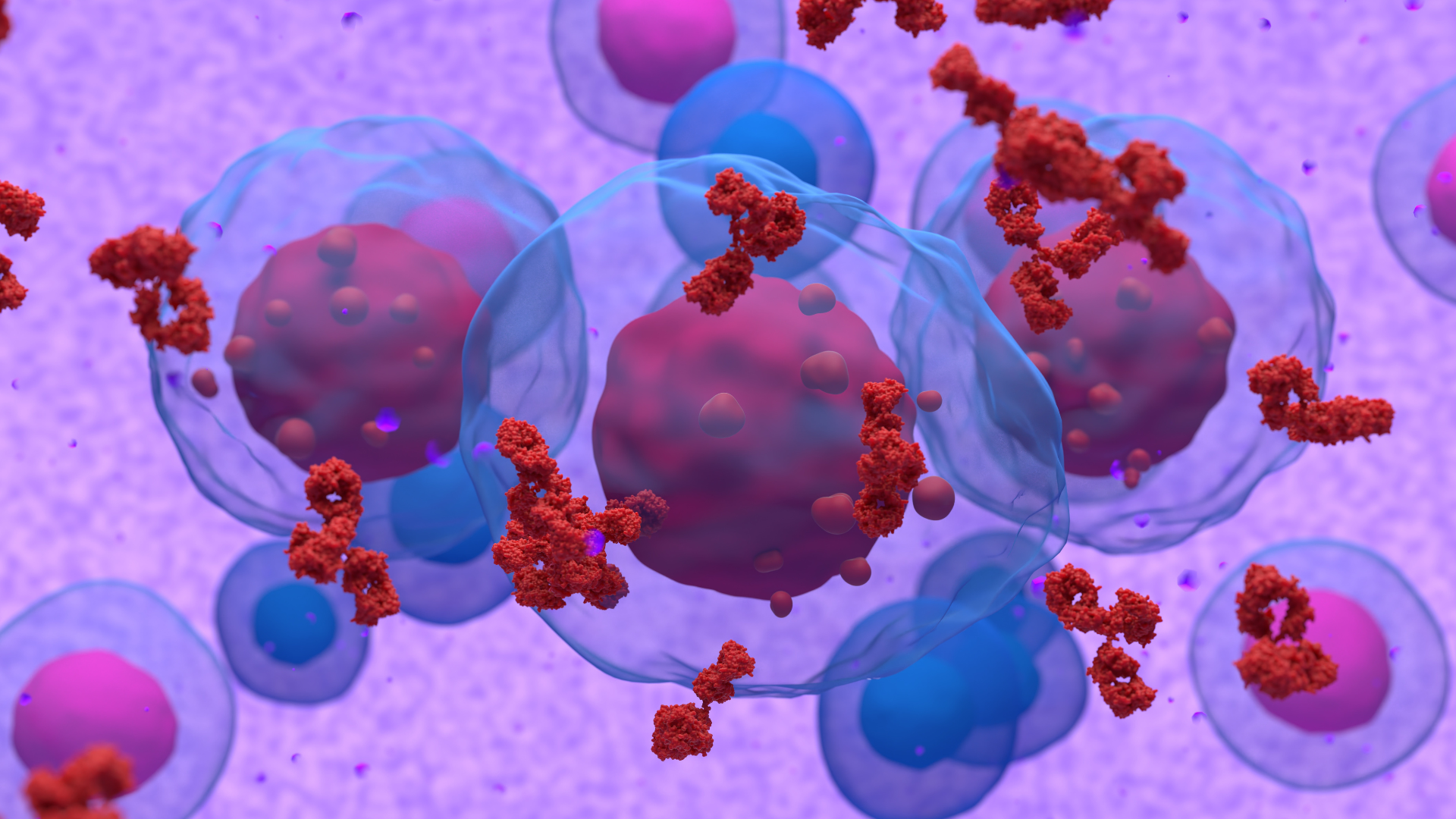
CAR T-cell therapy involves reprogramming a patient’s T-cells to target and destroy cancer cells. For example, ciltacabtagene autoleucel (Carvykti; cilta-cel), a BCMA-directed CAR T-cell therapy, has shown impressive efficacy in clinical trials. Despite its promising results, the therapy is associated with significant adverse effects, primarily cytokine release syndrome (CRS) and neurotoxicity.
CRS is an acute inflammatory response caused by the rapid activation of CAR T-cells, leading to the release of cytokines. Symptoms range from mild flu-like symptoms to severe, life-threatening reactions such as high fever, hypotension, and respiratory distress. Neurotoxicity, on the other hand, can manifest as confusion, aphasia, seizures, and, in severe cases, cerebral edema.
The Role of Oncology Nurses in Managing CRS
Early detection and prompt management of CRS are crucial for patient safety. Standard premedications, such as acetaminophen and antihistamines, are administered to mitigate mild symptoms. For moderate to severe CRS, interventions include the administration of tocilizumab (Actemra), an IL-6 receptor antagonist, and corticosteroids. Oncology nurses must be adept at implementing these protocols and collaborating with the healthcare team to provide timely care.
Neurotoxicity presents another significant challenge in CAR T-cell therapy. Oncology nurses conduct regular neurological assessments to detect early signs of neurotoxicity. In cases of severe neurotoxicity, interventions may include corticosteroids, anti-seizure medications, and supportive care in an intensive care setting. Continuous monitoring and timely communication with the medical team are essential to manage these complex cases effectively.
Educating and Supporting Patients and Families
Patient education is a fundamental aspect of managing patients during and after CAR T-cell therapy. Oncology nurses are responsible for preparing patients and their families for the potential adverse effects of the treatment.
Nurses educate patients about the signs and symptoms of CRS and neurotoxicity, emphasizing the importance of reporting any changes immediately. This proactive approach enables early intervention and improves patient outcomes. Additionally, providing emotional support and counseling helps alleviate anxiety and fosters a positive treatment experience.
Education also becomes a critical component for other members of the healthcare team who may care for patients experiencing adverse effects from CAR T-cell therapy. This becomes a factor especially for patients who return to receiving care at community centers compared with larger institutions.
Continuous Education and Research
Staying updated on the latest developments in CAR T-cell therapy is crucial for oncology nurses. Participation in ongoing education and research enhances their ability to manage adverse effects effectively. Receiving this information to then disperse it to patients is important to prepare them for any potential scenarios with CAR T-cell therapy.
Multidisciplinary Training of BiTE-Associated AEs Increases Safety in Outpatient Setting
April 13th 2025Authors noted that BiTEs have expanded the treatment paradigms for several types of solid tumors and blood cancers; however, toxicities associated with this class of agents have raised safety concerns.



