Living With WM: 17 Years And Going Strong
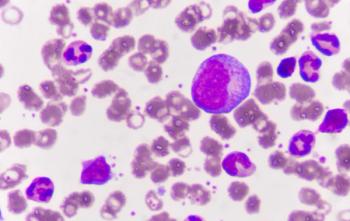
Marguerite Regan, PhD, was diagnosed with Waldenstrom's macroglobulinemia in 1995 and shares practical wisdom from her experiences, including reminding patients that WM isa treatable illness, not an end game.
Marguerite Regan, PhD, a resident of the Washington, DC area, was diagnosed with WM in 1995 at the time when Arnold Smokler, the founder of the IWMF, had formed the original support group—meeting a small number of WM patients in his home. Seventeen years later, Regan recounts the treatments that allowed her to continue her career and shares her practical wisdom with advice for those affected by a diagnosis of WM.
In January of 1995, I went to my internist with what I thought were gallbladder symptoms. She sent my blood to the lab for testing. At the lab they were unable to read the results. She took another test; the results also turned out to be unreadable. She talked about my case to a hematology colleague who thought he had an answer.
On February 9, 1995, I had a bone marrow biopsy. When I came out of the sedative, the hematologist informed me that I had Waldenstrom’s macroglobulinemia and I should rethink my life plans. At this time, WM had a five-year prognosis. I then went to the Johns Hopkins Hospital in Baltimore for a second opinion. Hopkins had a bone marrow transplant center and the hematologist there suggested I “upload all my risk factors and go for a transplant.” At this time, I was on watch-and-wait and bone marrow transplants had a very high mortality rate and their utility for WM was questionable. After a discussion with my hematologist, I decided against the transplant. I also adopted a dog as a life-affirming decision, and he was a good companion during the treatment times.
I was given Arnold Smokler’s name as someone who had WM and had researched it. Arnie was getting a support group together, so I attended a couple of those at his home. There were probably 4 to 5 of us in the beginning. Arnie had compiled a wealth of information on WM and it was good to know I was not alone. Later Arnie and his wife moved to Florida, and Sarasota became the center for WM information.
Watch-and-wait ended in 1999, when I was treated with cladribine (2CdA). I was in remission until summer 2004, when I had four sessions of Rituxan. That remission lasted until May of 2010, when I again had four sessions of Rituxan.
During these past 17 years I have been active with my work (at Envision EMI) as the curriculum director designing simulations for elementary through college students and as the Dean of Academic Affairs involved with accreditation. I traveled to various cities in the United States giving presentations and also abroad to Mexico, Jamaica, and Ireland, enjoying vacations. I plan to travel again this year. While I officially “retired” in January, 2011, I just signed a new consulting contract, good until 2014, for my company and am keeping busy at it.
Now I am faced with being treated once more for WM. I may seek a second opinion for the best combination of drugs, as well as discussing them with my hematologist-oncologist who has treated me for 17 years. Life with WM goes on. I also adopted another dog this month.
The most important lessons I learned during the last 17 years:
- View WM as a treatable illness, not an end game.
- Get a second or third opinion if necessary and find the best doctor to treat you.
- Be an advocate for yourself. Keep your records from diagnosis on.
- Keep your job if you are able to. I worked fulltime during most treatments (at Lombardi Cancer Center of the Georgetown University Medical Center), and it was a welcome diversion.
- Surround yourself with life-affirming people and stay away from naysayers.
- Gather your support group, be they family, friends, colleagues, dogs, cats.
- Divert your focus with creative projects and hobbies.
- Research information but do not over-focus on WM.
- Join a support group but remember that everyone may have different symptoms.
- Maintain your sense of humor, an important asset in dealing with any disease and with healthcare providers.
- Do not focus on “what-ifs” but stay in the present and seize the day.
Newsletter
Knowledge is power. Don’t miss the most recent breakthroughs in cancer care.