Innovative Use of Technology for Palliative Care
Innovative models for palliative care delivery and primary palliative care training are springing up to address the mismatch between the demand for this care and the capacity to deliver it.
Karen Ayers, ACHPN

Karen Ayers, ACHPN
With concern, you have just sent your patient home from the oncology clinic where you work. She’s just heard the results of her latest imaging studies and learned that her cancer has progressed, despite the efforts with first-line agents. You’ve seen her lose weight, slow down, and have trouble thinking and remembering things. You’re not sure how much support she has at home. You know that she’s been scheduled to start the second-line treatment soon. This is really taking a toll on her.
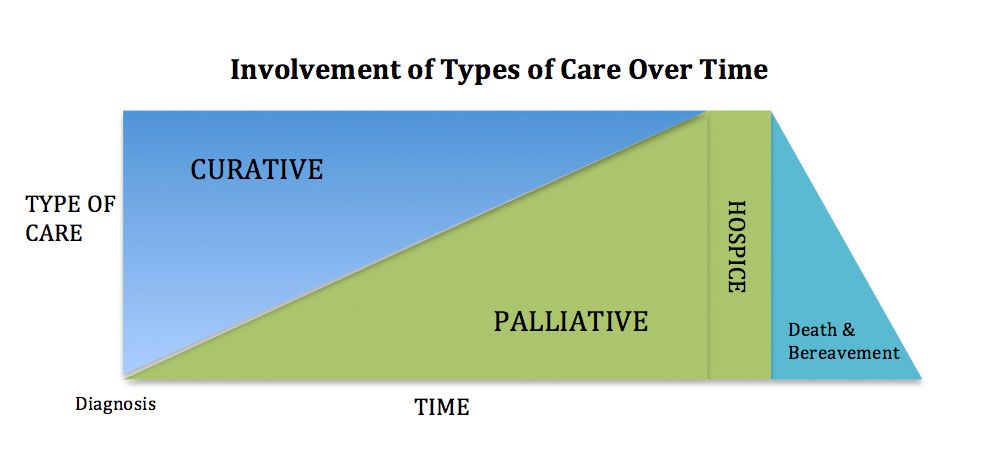
You think that a referral to palliative care is needed. But there are a couple of obstacles: first, you’re not sure how to explain what palliative care is, and second, the palliative care clinic is an hour’s drive away from where the patient lives, and the wait to get in to the clinic is 6 weeks.
This scenario is all too common. Unfortunately the demand for palliative care is high, and the capacity to provide it is low. As we know, our population is growing older faster. It is estimated that by 2030, more than 20% percent of US residents are projected to be aged 65 and older, compared with 13% percent in 2010 and 9.8% in 1970.1
As for workforce capacity, in California for example, a 2012 report estimated that of the approximately 100,000 physicians a little more than 900 were certified in palliative care (0.9%), and of the 262,000 nurses, 3800 worked in palliative care and just 789 of those had a certification in the field (0.3%).2
Recognizing the potential benefit of palliative care for so many of our patients, but its limited availability, new questions arise.
- How do we deliver more palliative care with available resources?
- How do we expand the resource pool of palliative care?
Nursing’s emphasis on the bio-psycho-social-spiritual wellbeing of people positions it perfectly to bridge the capacity gap in palliative care. Accordingly you will find nurses prepared at all levels as members of nearly all palliative care teams.
Extending Patient Access
Palliative care teams made their debut in acute care hospitals and more recently have extended into the outpatient setting. The usual arrangement is a clinic where the patient comes in for an appointment. Given that palliative care’s population is by definition burdened by serious illness, getting to a clinic—or making it to yet another appointment—can be very difficult and distressing. Many patients live far from a palliative care clinic or essentially have none available in their vicinity.
A recent California HealthCare Foundation publication about community-based palliative care includes a section on innovative models in palliative care.3 These models strive to improve the support and monitoring of patients and caregivers as well as to improve communication between patients and providers and among family members. They use a variety of technologies including remote monitoring devices, telephone, videoteleconferencing (VTC), and mobile devices. They have had many successes and also noted various challenges. Palliative care is a time- and detail-intensive service, no matter how it is delivered.
ResolutionCare, based in rural northern California, is taking a new approach to palliative care in the community. Rather than through a traditional “brick and mortar” clinic, a multidisciplinary team delivers care exclusively at home, either in person if the patient lives reasonably close to the administrative office or virtually by VTC if the individual lives farther away. The team manages many of the follow-up visits and urgent issues with a VTC connection and thus has been able to reach into remote “frontier” areas where no palliative care is otherwise available.
Meeting Training Needs
In addition to the problem of patients accessing palliative care, there remains the fact that there simply are not enough palliative care providers. ResolutionCare is addressing this challenge with an innovative teaching/learning model known as Project ECHO (echo.unm.edu).4 This “hub and spoke” model offers providers from underserved areas training, advice, and support in delivering best practice care for patients with complex health conditions, such as patients needing palliative care.
ResolutionCare invites learning “spoke” teams of physicians, advanced practice providers, nurses, and community health workers in rural northern California to join in biweekly VTC sessions with its palliative care team “hub.” They participate in a short didactic session followed by case presentations by the “spokes” to the VTC group of expert hub and learning spokes. As the hub at ResolutionCare offers advice and recommendations to the spoke presenting the case (and the spokes, in turn, feed back to the VTC group their successes and thoughts), all spokes learn. Those learners are becoming experts over time, and best practices are being developed. For those times when success is hard to see, the VTC group is there to offer support.
While it is widely recognized that palliative care is important to the wellbeing of those with serious illness and their families and caregivers, it is also evident that the capacity of palliative care as it stands today cannot possibly meet the demand. Fortunately, innovative models for palliative care delivery and primary palliative care training are springing up to address the demand—capacity mismatch—welcome news indeed.
Karen Ayers is a hospice and palliative care nurse practitioner at St. Joseph Hospital and Hospice of Humboldt in California. She is the program director at ResolutionCare.
References
- Ortman JM, Velkoff VA, Hogan H. An Aging Population: The Older Population in the United States. Current Population Reports. Washington, DC: US Census Bureau; May 2014. https://www.census.gov/prod/2014pubs/p25-1140.pdf.
- Rabow M. Palliative Topics in Healthcare: Chronic Illness & End-of-Life Care Through a Palliative Care Lens. California Quality Collaborative Symposium; January 14, 2015; Oakland, CA.
- Meyers K, Kerr K, Cassel B. Up Close: A Field Guide to Community-Based Palliative Care in California. www.chcf.org/~/media/MEDIA%20LIBRARY%20Files/PDF/U/PDF%20UpCloseFieldGuidePalliative.pdf. Accessed June 16, 2015.
- Arora S, Thornton K, Murata G, et al. Outcomes of treatment for hepatitis C virus infection by primary care providers. N Engl J Med. 2011;364(23):2199-2207.



