Daratumumab Approved Early by FDA for Multiple Myeloma
The FDA granted an accelerated approval of the CD-38-targeted monoclonal antibody daratumumab (Darzalex)-the first monoclonal antibody to be approved for patients with multiple myeloma.
DESCRIPTION
The FDA granted an accelerated approval of the CD-38-targeted monoclonal antibody daratumumab (Darzalex)—the first monoclonal antibody to be approved for patients with multiple myeloma.
Based on data from two open-label clinical trials, daratumumab was approved 4 months ahead of schedule as a monotherapy for patients who have tried at least three prior therapies.
In the phase II MMY2002 study, daratumumab demonstrated a 65% one-year overall survival (OS) rate and a 29.2% objective response rate (ORR). In the phase I/II GEN501 study, the ORR was 36%, median progression-free survival (PFS) was 5.6 months (95% CI, 4.2-8.1), and the one-year OS rate was 77% (95% CI, 58-88).
“Targeting proteins that are found on the surface of cancer cells has led to the development of important oncology treatments,” Richard Pazdur, MD, director of the Office of Hematology and Oncology Products in FDA’s Center for Drug Evaluation and Research, said in a statement. “Darzalex provides another treatment option for patients with multiple myeloma who have become resistant to other therapies.”
The decision follows a breakthrough therapy designation and a priority review, allowing for an approval based on ORR as a surrogate endpoint.
In MMY2002 study,1 the first 34 patients enrolled received daratumumab at 16 mg/kg (n = 16) or 8 mg/kg (n = 18). After a response evaluation, the 16 mg/kg dose was selected for future study, with an additional 90 patients enrolled at this dose. Data from the 106 patients who received the 16 mg/kg dose were used to support the approval.
Patients in the trial had received a median of five prior therapies over a median of 4.8 years following diagnosis. Ninety-six percent of patients were refractory to their last treatment, including proteasome inhibitors and immunomodulatory agents (IMiD).
Responses to daratumumab consisted of stringent complete responses (sCR; n = 3; 2.8%), very good partial responses (VGPR; n = 10; 9.4%), and partial responses (PR; n = 18; 17%). The median duration of response was 7.4 months. After a median follow-up of 9.4 months, 45.2% of patients remained on therapy. The median PFS was 3.7 months (95% CI, 2.8-4.6).
Infusion-related reactions (IRR) predominately occurred during the first infusion and were mostly grade 1/2 (all-grade 42.5%). Grade 3 IRRs were seen in 4.7% of patients; however, no grade 4 events were experienced. No patients discontinued daratumumab as a result of an IRR.
The most common all-grade adverse events (AEs) were fatigue (39.6%), anemia (33%), nausea (29.2%), thrombocytopenia (25.5%), back pain (22.6%), neutropenia (22.6%), and cough (20.8%). Overall, 4.7% of patients discontinued treatment due to AEs that were not deemed to be associated with daratumumab.
The GEN501 study contained two parts.2 In the first, 32 patients were treated with daratumumab at various doses, in order to find a recommended dose and schedule. In the second phase of the trial, 72 patients received daratumumab at either 8 mg/kg (n = 30) or 16 mg/kg (n = 42). In each group, patients had received a median of 4 prior therapies.
The median follow-up was 16.9 months in the 8-mg/kg group and 10.2 months in the 16 mg/kg arm. Patients who received daratumumab at 16 mg/kg experienced an ORR of 36%, which included 2 CRs and 2 VGPRs. Data from the 16 mg/kg arm were analyzed by the FDA for the approval.
ORR was higher in less heavily pretreated patients, at 56% for those who received 2 or 3 prior lines of therapy compared with 23% in a more heavily pretreated population. The estimated median duration of response in the 8-mg/kg arm was 6.9 months (95% CI, 6.2-10.6). In the 16-mg/kg arm, a median duration of response was not yet reached, with a one-year PFS rate of 65% (95% CI, 28-86).
In this trial, the most frequently occurring all-grade AEs with daratumumab were fatigue, allergic rhinitis, and pyrexia. Grade 3/4 AEs occurred in 26% of patients in the 16-mg/kg arm of the study and in 53% of those treated with the 8 mg/kg dose. Serious AEs occurred in 40% and 33% of patients in the 8 and 16 mg/kg arms, respectively. IRRs occurred in 71% of patients.
The FDA recommended dose and schedule for daratumumab is 16 mg/kg weekly for 8 weeks followed by every 2 weeks for 16 weeks and then once every 4 weeks until disease progression. Additionally, the agency noted that daratumumab interferes with blood bank crossmatching, specifically with indirect antiglobulin tests, warranting extra consideration when pursuing a blood transfusion.
“The responses we saw in clinical trials that led to today’s approval were striking, especially considering that these patients received a median of five prior lines of therapy,” Sagar Lonial, MD, chief medical officer, Winship Cancer Institute of Emory University and Professor and Executive Vice Chair, Department of Hematology and Medical Oncology, Emory University School of Medicine, said in a statement. “It appears the mechanism of action for daratumumab may play an important role in its single-agent activity among this group of advanced-stage multiple myeloma patients.”
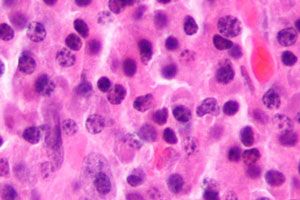
Daratumumab is a fully human monoclonal antibody that binds to glycoprotein CD38. Once bound, the antibody interacts with natural killer cells by mimicking the normal interaction between CD38 and CD31. This interaction elicits antibody-dependent cellular cytotoxicity and complement-dependent cytotoxicity resulting in antitumor activity.
A full indication for daratumumab is contingent on confirmatory studies, which are currently ongoing. The indication for daratumumab is specifically for patients following progression on a proteasome inhibitor and an IMiD or for those who are double refractory to a proteasome inhibitor and IMiD.
“Multiple myeloma is a highly complex disease and remains incurable, with almost all patients relapsing or becoming resistant to therapy,” Paul G. Richardson, MD, clinical program leader and director of Clinical Research, Jerome Lipper Multiple Myeloma Center, Dana-Farber Cancer Institute, said in a statement. “With Darzalex, we have a promising new immunotherapy, which has shown pronounced efficacy as a single agent with an acceptable adverse event profile. This is especially important for treating these heavily pre-treated patients in whom all of the major classes of currently available medicines have failed.”
In addition to single-agent activity, daratumumab is also being explored in a number of combination studies. At this time, several phase III clinical trials are looking at the antibody in various treatment settings.
References
1. Lonial S, Weiss BM, Usmani SZ, et al. Phase II study of daratumumab (DARA) monotherapy in patients with ≥ 3 lines of prior therapy or double refractory multiple myeloma (MM): 54767414MMY2002 (Sirius). J Clin Oncol. 2015;33 (suppl; abstr LBA8512).
2. Lokhorst HM, Plesner T, Laubach JP, et al. Targeting CD38 with Daratumum2ab Monotherapy in Multiple Myeloma [published online August 26, 2015]. N Engl J Med. doi: 10.1056/NEJMoa1506348
Shared Model of Care Post-HCT Offers Safe Follow-Up, Reduces Patient Burden
Published: March 19th 2025 | Updated: March 19th 2025Alternating post-HCT care between specialized facilities and local cancer centers produced noninferior non-relapse mortality and similar quality of life to usual care.


