Black Patients With Breast Cancer Experience Higher Rate of Treatment Modifications or Discontinuations
Treatment modifications were inconsistent among White and Black patients with breast cancer. However, the use of a multiscale biophysical modeling platform may be useful in informing treatment modification decisions.
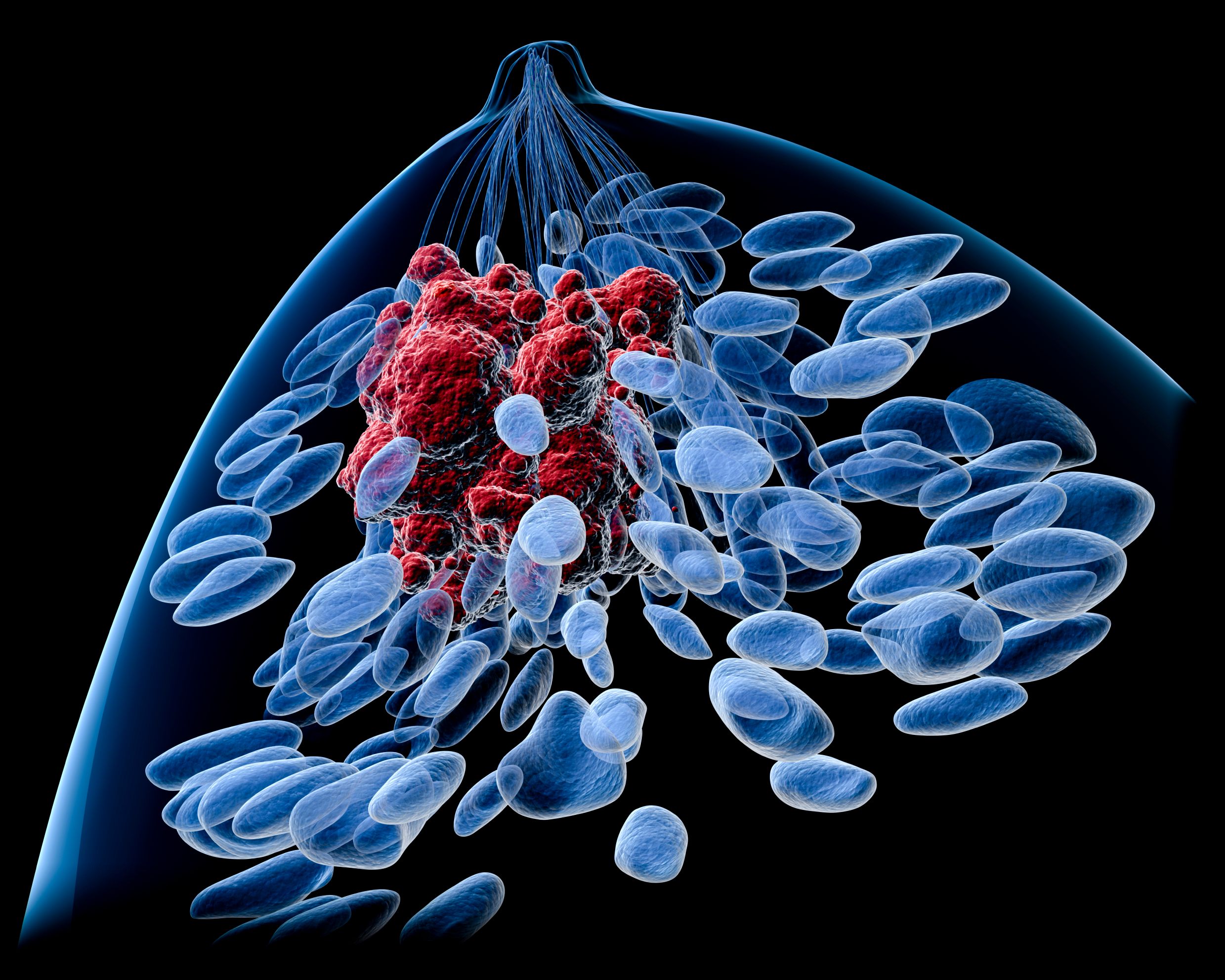
There is a higher incidence of treatment modifications or discontinuations in the neoadjuvant setting among Black patients compared with White patients who are receiving treatment for breast cancer, according to findings that were presented during the 2021 San Antonio Breast Cancer Symposium (SABCS).1
However, results from this proof-of-concept study demonstrated that the use of a multiscale biophysical modeling platform may help identify what treatment outcomes may look like before clinicians and patients decide whether to modify their current treatment.
Researchers conducted a retrospective review of 173 patients who had received neoadjuvant therapy from January 2010 through March 2020 and separated the patients into 2 cohorts: 114 who received a scheduled regimen (SR) and 59 who received a modified regimen (MR). Although there were nearly double the amount of patients in the SR group than in the MR cohort, Black patients accounted for 59% of the MR cohort.
In the MR group, a significantly lower proportion of patients achieved a pathologic complete response (pCR) compared with the SR group (odds ratio, 0.44; P = .03). Moreover, similar to what has been observed in other studies, 42% of Black patients had treatment interruptions compared with 25% of White patients.
“During neoadjuvant therapy in breast cancer, treatment interruptions may impact rates of pathologic complete response and ultimately increase risk of recurrence,” the study authors wrote in their poster at SABCS.
Six patients (10%) had early discontinuation of doxorubicin and cyclophosphamide, 25 patients (42%) had an early discontinuation of a taxane therapy, 7 patients (12%) had an anti-HER2 therapy discontinued, and 21 patients (36%) had dose reductions throughout their therapy.
The study authors observed a pCR rate of 42% in the SR group and 20% in the MR group.
Utilizing the multiscale biophysical modeling platform, known as TumorScope, the researchers were able to use data from patients in the MR group and simulate what responses to treatment may have been if patients had received the full dose of their treatment uninterrupted. The simulation demonstrated that without treatment interruption, 10 additional patients (5.6%) would have been able to achieve a pCR. In the simulation, 100% of patients receiving SR had a complete response in comparison with 81.7% of those who would experience treatment interruptions.
TumorScope was previously evaluated in a separate study to determine its effectiveness and was used in several other studies and analyses presented at this year’s SABCS.2 According to the study researchers, the results show that TumorScope can be used to estimate the impact of variable dosing before clinicians decide to interrupt a patient’s treatment. Furthermore, researchers believe that TumorScope can evaluate individual treatments being considered for this patient population to support de-escalation of therapy ahead of time but note that further study is needed.
References
- Pandey T, Pfeiffer J, Braun E, at al. Assessing the impact of treatment interruptions during neoadjuvant therapy in early stage breast cancer. Presented at: 2021 San Antonio Breast Cancer Symposium; December 7-10, 2021; San Antonio, TX. Abstract P1-08-21.
- SimBioSys presents new studies on its precision medicine software platform at the 2021 San Antonio Breast Cancer Symposium. News release. SimBioSys. December 1, 2021. Accessed December 8, 2021. https://bwnews.pr/3oz8qAP


