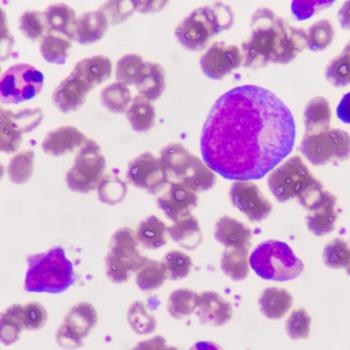
Myeloproliferative Neoplasms
Latest News
Latest Videos
More News
Both those receiving either expected or less-than-expected starting dosages of ruxolitinib for myelofibrosis treatment reduced daily dosages over 12 months.

Clinical response rates were higher in patients with phlebotomy-dependent polycythemia vera who received rusfertide than in those who received placebo.

Ropeginterferon alfa-2b showed superior efficacy over anagrelide in the SURPASS-ET trial for essential thrombocythemia, with higher durable response rates and greater JAK2 allele burden reduction.

The combination of selinexor with ruxolitinib, in both 40mg and 60mg doses, demonstrated encouraging efficacy with a manageable safety profile in patients with myelofibrosis.

Most patients with lower-risk myelofibrosis, over a 4-year period, experienced disease progression, as demonstrated by the prospective MOST study.

Updated data from the MANIFEST-2 study support a paradigm shift in the treatment of JAK inhibitor–naive patients with myelofibrosis.

Patients with phlebotomy-dependent polycythemia vera, a type of myeloproliferative neoplasm, treated with rusfertide experienced greater responses compared with those treated with placebo.

The FDA has approved momelotinib (Ojjaara) for the treatment of adult patients with intermediate or high-risk myelofibrosis, including primary myelofibrosis or secondary myelofibrosis, and anemia.

Jaktinib is a novel JAK and AVCR1 inhibitor that showed activity in patients with myelofibrosis who were intolerant to or progressed on ruxolitinib.

For patients with myelofibrosis receiving pacritinib, spleen volume reduction was associated with improved overall survival.
Onco-Nursing Experts Define Best Practices, Treatment Considerations for Managing Patients With MPNs
Specialists highlight the best practices and latest treatment regimens for patients presenting with myelofibrosis, polycythemia vera, and essential thrombocythemia.

After 6 months of treatment with ruxolitinib, patients with polycythemia vera experienced a significant reduction in hematocrit levels compared with baseline.

Following treatment with rusfertide, patients with polycythemia vera were able to significantly reduce their need for blood draws.

Pacritinib helps relieve physical function-related symptoms in adult patients with myelofibrosis and moderate or severe thrombocytopenia.

An expert with Oregon Health & Science University discusses whether Orca-T graft can fulfill an unmet need in the field of allogeneic stem cell transplantation for myelofibrosis.
An expert from Mount Sinai Hospital comments on potential new ruxolitinib combinations to treat patients with myelofibrosis and MPNs.

Ruxolitinib was not associated with an increased risk of secondary malignancies in patients with polycythemia vera.

Treating patients with myeloproliferative neoplasms in accelerated phase (MPN-AP) remains an ongoing challenge as there are still no standard therapeutic approaches, says an expert.

Allogeneic hematopoietic stem cell transplant (HSCT) is still the sole curative therapeutic modality for patients with myelofibrosis.

Despite relatively good cardiovascular health, a significant percentage of patients with MPN were not prescribed appropriate medication.

The phase 3 SIMPLIFY 1 and SIMPLIFY 2 trials reported that Week 24 transfusion independence resulted in an improved overall survival for patients with myelofibrosis.

Novel therapeutics have not only boosted outcomes in myelofibrosis, but paved the way for new combination treatment strategies, too.

Combinations of JAK inhibitors and novel agents, such as epigenetic regulators, could help prolong survival in patients with myeloproliferative neoplasms.

With additional JAK inhibitors under exploration in the myelofibrosis pipeline, such as momelotinib and pacritinib, FDA-approved options continue to be utilized heavily in the paradigm, explained John O. Mascarenhas, MD.

A rolling submission of a new drug application (NDA) for the JAK2/FLT3 inhibitor pacritinib has been initiated for patients with myelofibrosis and severe thrombocytopenia defined as platelet counts of less than 50,000 μL.