1 in 5 Patients Engage in Nonmedical Opioid Use
Nearly 20% of patients with cancer engaged in nonmedical opioid use, but oncology nurses can help prevent this from happening.
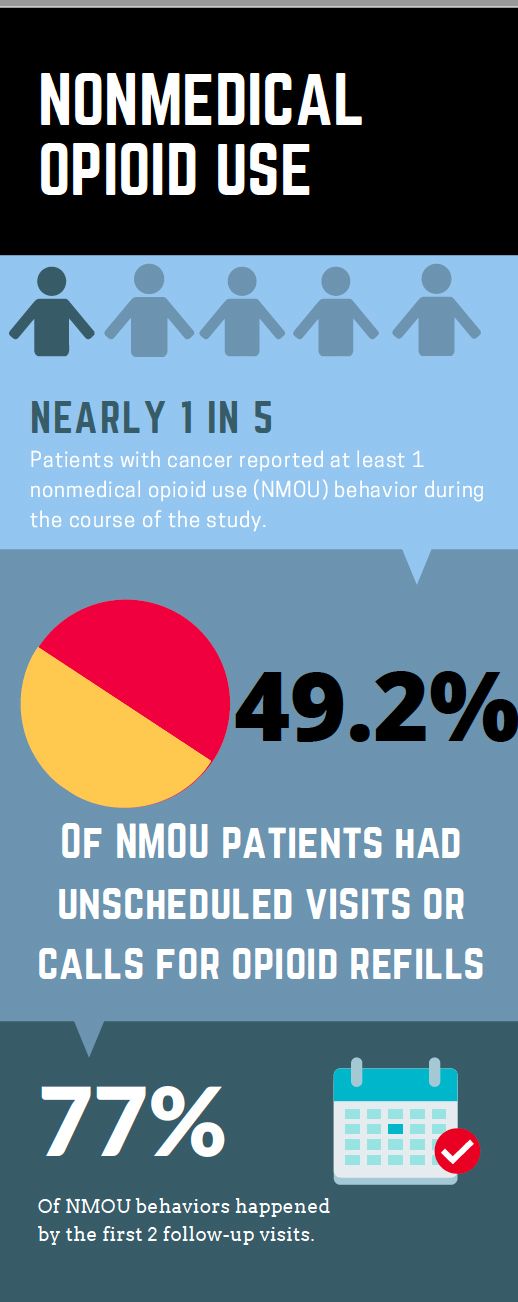
Nearly 1 in 5 patients with cancer engaged in nonmedical opioid use (NMOU), though there are certain risk factors that nurses can look out for to help determine who is more at risk, according to recent research published in JAMA Oncology.
Researchers evaluated 1554 patients with cancer being treated at The University of Texas MD Anderson Cancer Center (MD Anderson) who were taking an opioid for cancer-related pain at least once a week.
Participants had their pain levels, social statuses, and other factors measured through a series of scales, such as the Screener and Opioid Assessment for Patients with Pain (SOAPP), which rates relationships, medication-related behaviors, substance abuse history, doctor-patient relationships, and psychiatric and neurobiological need for medicine.
“Now that there is this epidemic of opioid misuse and opioid addiction, it’s a very important thing to learn about: how these patients have cancer but are also at risk for opioid misuse. What are the complications? What are the consequences? How can we help them?” said Sriram Yennu, MD, MS, FAAHPM, study author and professor in the department of palliative care and rehabilitation medicine at MD Anderson.
A total of 19.2% of participants engaged in NMOU, with the most common, by far, being frequent or unscheduled clinic visits or phone calls for refills, which occurred in 49.2% of patients with 1 or more NMOU behavior. One explanation behind this, Yennu said, is that it was an objective item that the researchers could measure, unlike some of the others — such as using opioids that were not prescribed – which patients had to report themselves.
Other NMOU behaviors included self-escalation of opioid dose for excessive increase in the opioid dosage that is not consistent with the patient’s pain syndrome; use of nonprescribed restricted medications or illicit drugs; and reports of impaired functioning in daily activities due to opioid use.
The researchers found that the following factors were independently associated with NMOU behavior:
- Marital status: Single patients were more likely to engage in NMOU.
- SOAPP score: Patients scoring 7 or higher were at greater risk.
- Morphine equivalent daily dose: 50mg or higher was associated with increased risk.
- Edmonton Symptom Assessment Scale pain level.
Yennu emphasized that nurses can lead the way in preventing NMOU, by using validated tools to assess patients’ pain and their opioid use.
“The best thing you can do to help the patient is to follow up with the patient more, and only give a small amount of opioids,” he said. “So rather than give a prescription for opioids for 1 or 2 months, [opt for] a shorter prescription and more follow up, in addition to helping the patient find counseling and other resources.”
These findings lay the groundwork for future research, as well as potential changes in cancer clinics across the nation. The researchers stated that universal screening, setting limits on opioid use, and implementing more intense follow-up with an interdisciplinary team can help ensure that patients are safely managing their symptoms.
“This is just the tip of the iceberg, and there is still a lot to be learned about,” Yennu said. “We need to think first about the patient, how we can make their life better, especially if they are in pain.”


